There are ~ 280k THA per year, 4.1% revision risk at 5 years [1]. Most common reason is instability (22.5%), loosening (19.7%), infection (14.8%) [2].
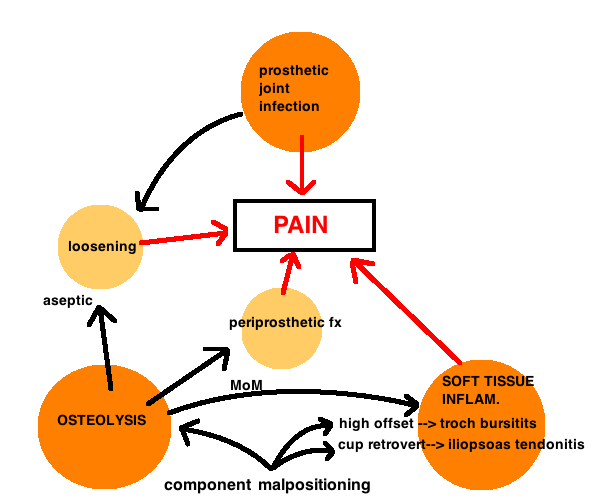
Pain is the most common symptom for nearly all complications after THA, and therefore pain is best evaluated algorithmically.
Pain over greater troch (troch bursitis?, maybe too much offset), pain with hip flexion (iliopsoas tendonitis?, maybe too little anteversion); start up pain (loosening?: thigh pain is stem loosening, deep buttock or groin pain is acetabular); pain at all times of the day (infection?). Maybe no improved pain since surgery, consider extrinsic causes (back or knee, peripheral vascular disease, sciatic nerve irritation, meralgia paresthetica, malignancy). Persistent pain since surgery could also be intrinsic (infection, unstable implant – failed integration, malpositioned component).
On exam. Watch the gait. Limp? Due to muscle weakness or pain or LLD. Abductor deficiency is seen most commonly with the direct lateral approach. When considering LLD, watch out for a fixed pelvic obliquity from adductor contractures or spinal disease which cause apparent, not true LLD. Look at the incision for signs of warmth, redness. Take the leg through ROM to look for instability or impingement. Pain with resisted hip flex is iliopsoas tendonitis.
Thigh pain is a symptom seen in loosening (secondary to osteolysis, infection) and in some cases of press fit THA. The pain is anterolateral and mid-thigh (corresponding to the level of the stem tip). The cause of pain in press-fit THA is imperfectly understood but thought to be associated with the mismatch between implant and bone modulus of elasticity…larger stem sizes, stainless steel stems, straight designs are more rigid [3]. Thigh Pain is treated nonoperatively for 18 – 24 months before considering surgery, and yet stem revision for unknown pain is controversial[4] . Surgery involves cortical strut graft with cerclage wiring to host bone while retaining the femoral stem (if its well fixed) [5]. The strut increases the rigidity of the host bone and decreases the modulus mismatch of the implant and host bone. Results are successful.
REFERENCES
1. Bozic, K.J., et al., Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res, 2010. 468(9): p. 2357-62.
2. Bozic, K.J., et al., The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am, 2009. 91(1): p. 128-33.
3. Lavernia, C., et al., Thigh pain in primary total hip arthroplasty: the effects of elastic moduli. J Arthroplasty, 2004. 19(7 Suppl 2): p. 10-6.
4. Brown, T.E., et al., Thigh pain after cementless total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg, 2002. 10(6): p. 385-92.
5. Kim, Y.H. and J.S. Kim, Revision hip arthroplasty using strut allografts and fully porous-coated stems. J Arthroplasty, 2005. 20(4): p. 454-9.