1. HISTORY OF TKA
1861: Dr. Fergusson performed resection arthroplasty of knee for arthritis. This was followed in 1863 by Dr. Verneil with interposition arthroplasty, which inserted foreign tissue (including capsule, skin, muscle, fat chromatized pig bladder) into the joint. This technique failed to provide lasting pain control.
1940s: Knee Hemiarthroplasty: Dr.Campbell was using a variation of the aforementioned technique (using free fascial graft), when he heard about Smith-Perterson’s success using mold arthroplasty for the hip. Campbell performed a mold hemiarthroplasty of the knee by fitting metallic molds to the femoral condyles. This technique failed to provide pain relief, however, the technique was modified by Smith-Peterson, who added a stem to the the prosthesis, and this allowed some very short-term success (called the Massachusetts General Hospital Femoral Condylar Replacement). During this same time period, Drs. McKeever & MacIntosh developed a tibial hemiarthroplasty, using vitallium (the same material being used for hip hemiarthroplasty at the time), which failed due to early loosening.
MacIntosh was also very important to the progress of TKA by developing many of the instruments necessary to reliably reproduce TKA. As you notice from this section, there is a huge emphasis on implant design, yet the bone cuts required for accurate and reproducible TKA is equally challenging as making good implants. He came up with the concept of creating flexion and extension gaps, and using spacers to measure and achieve ligament balance.
1950s: Walldius Shiers attempted the first bicompartmental knee arthroplasty (replacing both the femur & tibial articular surface) using a hinge with intramedullary stems. The initial design experienced a high loosening rate, and a follow up design called the GUEPAR hinge was developed, which shifted the axis of rotation posteriorly. This design still failed due to loosening as it failed to account for the complex rotational motion of the native knee.
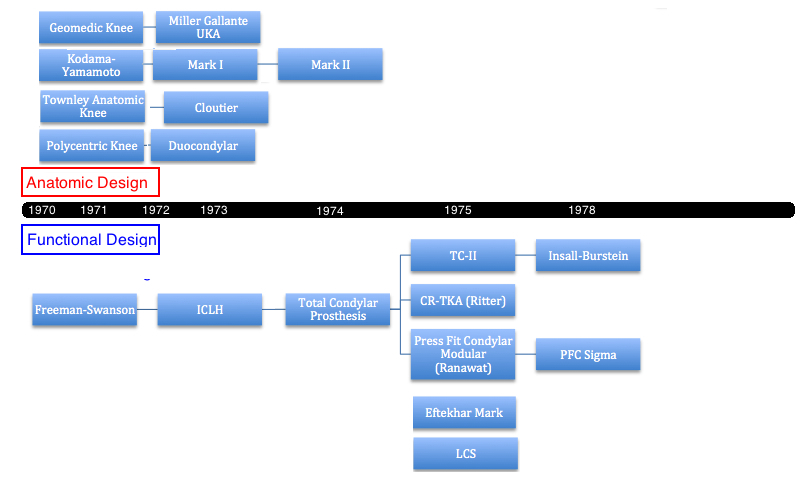
1970s: The 1970s were a turning point for knee arthroplasty. The first designs that lay a foundation for current implants were developed and many of the current concepts and technologies that were developed in the 70s are used today. There were two design theories that took hold. One design attempted to recreate the normal knee anatomy and thus recreate normal knee kinematics. The other design attempted to simply the process by making anatomy secondary to function. This design emphasized knee mechanics over all else. Over the past 30 years, the second approach, this mechanics over anatomy, became the predominant method for designing TKA. However, with increasing technologic and technical sophistication, the first design, that of re-creating native anatomy and kinematics, as regain interest as a means to improve TKA function and patient satisfaction.
Important advances in material science proceeded this rapid development in TKA design. The original polyethylene (“high density plastic”) was developed in 1963. The bone cement methylmethacrylate was approved for medical devices by the FDA in 1971. Furthermore, advances in total hip arthroplasty, notably pioneered by Dr. John Charnley, occurred just prior to the 1970s, and many of the theories were applied to TKA.
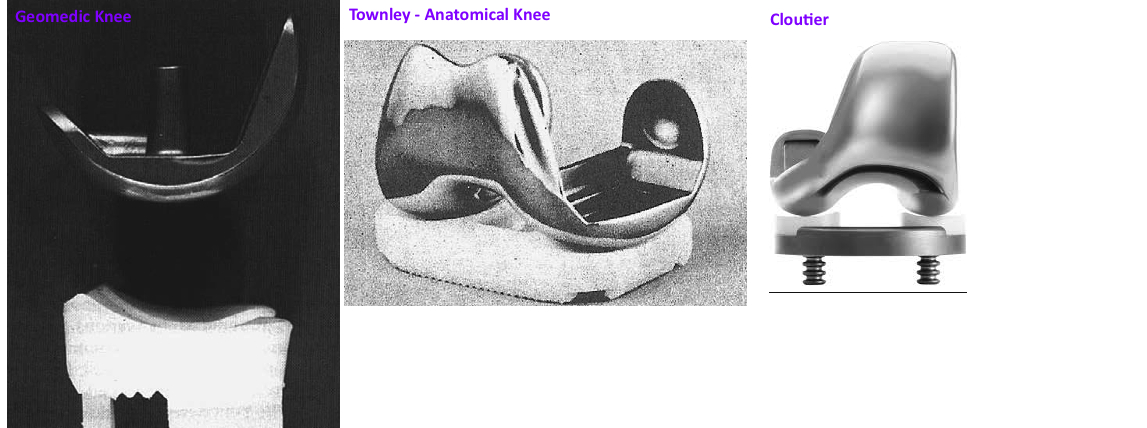
1971: The first bicompartmental knee arthroplasty without a hinge for stabilization was the Polycentric Knee developed by Dr. Gunston, who had previously studied in Dr. John Charnley's lab. The design recognized that knee kinematics do not occur in a single plane like a hinge, rather the femoral condyles roll/glide with a changing center of rotation throughout the arc of motion. This was the first design that did not attempt to reconstruct the knee as a "hinge" but rather attempted to preserve knee anatomy (kept the cruciate and collateral ligaments). The procedure resurfaced the femoral condyles and cemented separate cobalt-chrome semicircular implants using polymethylmethacrylate (PMMA). On the tibial side, the medial and lateral tibial compartments were resurfaced and cemented in two concave polyethylene liners. This was an Anatomic Design. This design provided short-term pain relief, survivorship was significantly improved, however the implants failed due to inadequate fixation to the bone.
Other Anatomic design TKA were developed around the same time. The Kodama-Yamamoto knee was a metal femoral implant with a single polyethylene mold for the tibial side that was minimally constrained and had a central cutout for the cruciate ligaments. This implant was modified further as the Mark I and Mark I and demonstrated fairly good survivorship. Dr. Townley designed the Total Knee Original. The femoral implant had a decreasing radius of curvature to encourage femoral rollback, and a single polyethylene tibial implant. This model was the foundation for future anatomic designs such as the Cloutier, and Natural Knee.
Dr. Coventry, at the Mayo Clinic, developed the Geomedic knee in conjunction with Mr. Averill (engineer at Howmedica) . The Tibial component was solid polyethylene and conformed closely to the femoral component. It preserved the cruciate ligaments . However, due to the highly conforming articular geometry, in combination with cruciate preservation, there was a kinematic conflict that lead to early loosening. The implant was not a hinge, but the motion was too restricted. It was recognized that articular geometry and surrounding soft tissue both guide knee motion, yet, both cannot strongly guide motion otherwise there is conflict. While the design was generally considered a failure, derivations of its design were continued by Zimmer, and lead to successful implants such as the Miller-Gallante unicondylar knee, which is considered the first successful UKA. The Nextgen by Zimmer is also a variation of the Geomedic.
1970: Drs. Michael Freeman (surgeon) and SAV Swanson (Professor of Mechanical Engineering) developed the Freeman-Swanson bi-compartmental knee prosthesis, which is truly the first iteration (the fountainhead) of the current TKA, in both theory and design. In theory, the goal of the implant was to emphasize mechanical stability and prioritize function over preservation of anatomy. Dr. Freeman recognized that many of the knees requiring arthroplasty had significant angular deformity and therefore he decided that mechanical alignment was best achieved by sacrificing the cruciate ligaments. The implants were placed for mechanical alignment, not anatomic alignment.
Furthermore, without cruciate ligaments, the tibial eminence could be removed, offering multiple advantages. Instead of making many small bone cuts to reproduce the complex knee anatomy, simple parallel bone cuts could be made (one across the entire tibia) to facilitate the surgery and thus its reproducibility. Freeman introduced the idea of creating parallel cuts in the knee, perpendicular to the mechanical axis. He introduced intramedullary guides to achieve proper angulation of these cuts.
Freeman employed MacIntosh’s concept of spacer blocks for gap balancing. Laminar spreaders were first used for ligament balancing by Freeman after a visit from a South African doctor: Van Vuren. Freeman essentially standardized the basic steps for TKA (with one interesting difference. For the final implants he put the femur first, and then slid the tibial component into place like pushing a drawer back into a dresser).
The other advantage of removing the cruciates and the tibial eminence, was that a single cut across the tibia gives a larger bone surface area for the tibial implant, which then allows for a larger implant with better distribution of joint forces. However, Freeman later realized that removal of the tibial crest without replacing it with a tibia post, allowed for medial-lateral instability that caused implant failure.
Removing the cruciate ligaments also simplified the TKA kinematics. Implant stability and kinematics depended not on the surrounding soft tissue but rather through highly constraining articular geometry (concave tibial component). The femoral condyles were simplified to a single radius of curvature that matched the tibia. There was no posterior rollback, rather the kinematics were described as a “roller-in-trough” design.
The femoral component was made of cobalt-chrome. The tibial component was made of polyethylene. And there was just one implant size!
The patellofemoral joint was not addressed. The femoral component lacks an anterior flange.
1973: Freeman and Swanson produced the next generation of their implant by added the anterior flange to the femoral component and a patellar button to resurface the patella. This implant was named the ICLH (Imperial College London Hospital).
The next generation of design was the Freeman-Samuelson Knee which developed a tibial post to provide improved medial-lateral stability.
1971: At the same time that Dr. Freeman and associates were making great strides in the UK, a friend of his from medical school at Corpus Christie College in Cambridge UK, Dr. John Insall, was working with Dr. Chitranjan Ranawat and Dr. Peter Walker at HSS to develop a total condylar knee. Their first design was the Duocondylar Knee. In contrast to the Freeman-Swanson, the Duocondylar knee was based on recreating knee anatomy and native kinematics by preserving the cruciate ligaments. The tibial component was two flat pads (one for the medial and one for the lateral compartment) which did not attempt to control kinematics nor provide stability. This design relied on native soft tissue balance. Early results from this implant indicated that preservation of soft tissue (particularly the cruciate ligaments) impeded the correction of many deformed knees, and preservation of the tibial eminence prevented sturdy implantation of the components.
1974: These same designers (Insall et al) took the lessons from the Duocondylar implant and focused their efforts on the alternative theory of design: functional TKA (similar to the Freeman-Swanson). They then developed the Total Condylar (TC) prosthesis at HSS, which was strongly influenced by the ICLH design, and was truly the first TKA with reliable and reproducible functional outcomes and long-term survivorship. Similar to the ICLH, the cruciates were sacrificed, the femoral condyles were symmetric yet unlike the ICLH, there was a more anatomic change in the radius of curvature posteriorly (there were 2x radii, smaller poteriorly). There was an anterior flange with a trough to help with patellar tracking (there was a patellar button). The tibial component was polyethylene that was partially conforming (a “double-dish” shape, which was less conforming than the ICLH) and a lip anterior/posterior to prevent dislocation. The tibial component additionally had a very short post to replace the tibial eminence and give some medial-lateral stability. This was a Cruciate Sacrificing Design (cruciates removed, no post to replace).
This design was an improvement on the ICLH by utilizing both articular geometry and soft tissue tension to provide stability and kinematic guidance. The first implant was done at HSS by Dr. Insall.
It was completely congruent in extension and flexion. The main issue was that the significant conformity and congruency of the tibial design prevented any femoral rollback and thus limited knee flexion, and there were some cases of posterior subluxation in flexion.
1975: Total Condylar II. Despite using semicongruent articular geometry and a small tibial eminence, instability was still a problem with the TC design. During flexion, the femur could sublux anteriorly. To address this instability, the TC II created a central tibial post to engage the femur in flexion and prevent anterior subluxation (early version of the posterior stabilized design), yet the increased forces encountered through this post lead to higher loosening rates and this model was not continued for long,although it was the first foray into PS-design. Other variations of the TC design, led by Dr. Ranawat, include the Press-Fit Condylar (PFC) and PFC Sigma (DePuy).
1974: Dr. Eftekhar was the first to design the metal tibial baseplate with variable tibial polyethylene inserts. His design joined with the Mark I design (a derivation of the Kodama-Yamamoto knee). The initial tibial poly inserts came in sizes 6, 10, and 15.
1975: At the same time the New Jersey Knee was developed by Dr. Pappas and Buechel, which was the first implant with a mobile bearing and rotating platform, and was called the LCS (low contact stress).
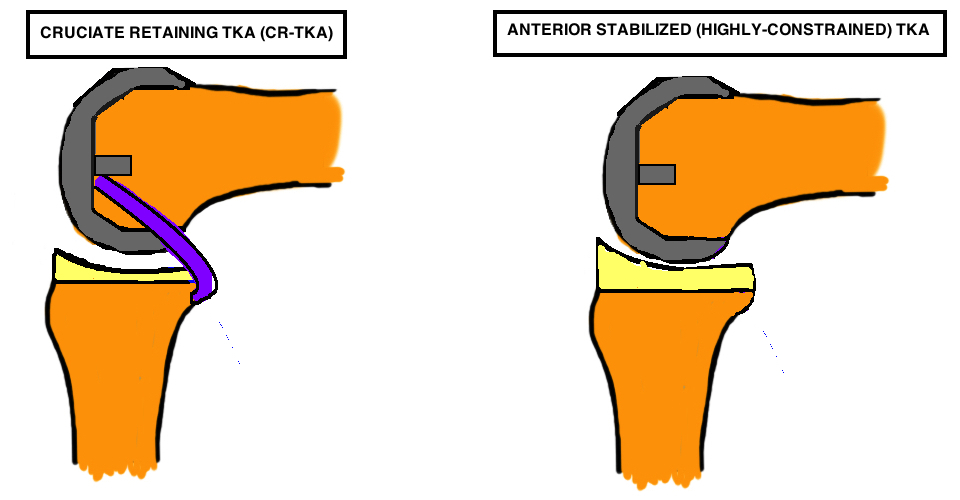
1975: An HSS-trained surgeon, Dr. Merril Ritter was introduced to the TC prosthesis and requested a variation to the tibial component: cut out a posterior inlet to allow for preservation of the PCL. This was the origin of the CR-TKA.
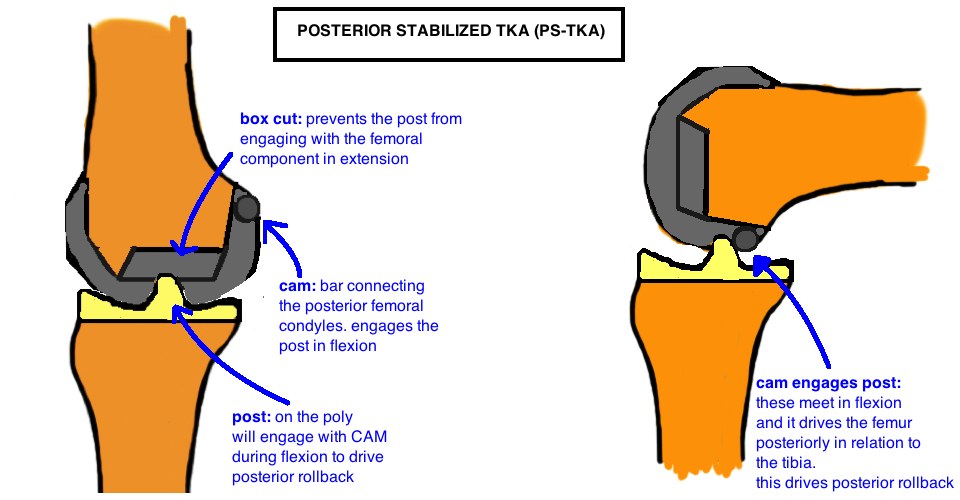
1978: The Insall-Burstein prosthesis corrected the limitations of the Total Condylar Prosthesis by creating the first Posterior-Stabilized design: a central cam on the femur which engaged the back of tibial post at 70° of flexion and drove the contact point posteriorly during flexion to create femoral rollback. Most of the current PS designs derive from this Insall-Burstein knee. The major limitation of the IB knee was the high incidence of patellar dislocation. Since then, an asymmetric anterior flange was developed (higher laterally) to improve patellofemoral tracking.
References
1. Gunston, F.H., Polycentric knee arthroplasty. Prosthetic simulation of normal knee movement: interim report. Clin Orthop Relat Res, 1973(94): p. 128-35.
2. Yamamoto, S., S. Nakata, and Y. Kondoh, A follow-up study of an uncemented knee replacement. The results of 312 knees using the Kodama-Yamamoto prosthesis. J Bone Joint Surg Br, 1989. 71(3): p. 505-8.
3. Goldberg, V.M. and B.T. Henderson, The Freeman-Swanson ICLH total knee arthroplasty. Complications and problems. J Bone Joint Surg Am, 1980. 62(8): p. 1338-44.
4. Insall, J., et al., Total condylar knee replacment: preliminary report. Clin Orthop Relat Res, 1976(120): p. 149-54.
2. Primary TKA Designs
The goal of all TKA designs is to provide stability, longevity and normal kinematics. The native knee relies on both articular congruence and soft tissue tension to guide motion. As discussed in the History of TKA, the competing designs for TKA were anatomic vs. functional. The superior reproducibility of the functional approach lead to it becoming the gold standard for TKA. Within this group, the Cruciate-Sacrificing (CS-TKA) was first developed (the ICHL and the Total Condylar), with further development leading to the Posterior-Stabilized (PS-TKA) design (Insall-Burstein and its later derivations), and the Cruciate-Retaining design (CR-TKA). There are many randomized-control trials and meta-analyses comparing the PS and CR designs without demonstrating superiority in patient satisfaction, function, pain, or complications.
The standard primary TKA is comprised of a cemented Cobalt-Chrome femoral component, a polyethylene liner and a titanium tibial baseplate, and polyethylene patellar button (if the patella is resurfaced), . The tibial component is not always a baseplate + liner, but rather can be a monoblock tibial poly (the poly liner is cemented directly onto the tibia without the tibial baseplate, and this monoblock tibia is significantly cheaper and has equal if not better longevity). The tibial component (poly liner + tibial base plate) starts at 9 mm thickness and can increase by 1 mm increments based on the amount of tibial bone resected. The tibial base plate is always about 2 mm thick, additional thickness comes from the poly. The poly thickness is labeled as 9 mm etc but that measurement incorporates the 2 mm of tibial tray, and represents the thickest part of the poly. In reality, the concavity of the liner is thinner, maybe 5-6 mm, and if any thinner, the poly risks fracture.
Posterior Stabilized (PS-TKA)
The Posterior-Stabilized TKA is designed with the goal of Mechanical Alignment. It relies on a tibial cut and femoral cuts that are perpendicular to the mechanical axis. The PS-TKA uses a Cam on the femur to engage to the back of the tibial Post (at 40 – 90° flexion) to push the femoro-tibial contact point posteriorly during knee flexion. This is “posterior rollback” and its essential for the knee to achieve deep flexion because terminal flexion occurs when the posterior femoral cortex impinges on the posterior tibial plateau (on the lateral side). By allowing the femur to rollback, it creates more offset before impingement occurs, enabling a deeper flexion. Historically, knee flexion in TKA was limited to 90° when there was no rollback (seen with the cruciate sacrificing TKA). The PS-TKA posterior rollback is only 80% of what is observed in the native knee. Yet in comparison to CR-TKA designs, it is generally considered to drive greater and more reliable rollback. Importantly this does not appear to influence functional outcome or even range of motion. Kinematic analysis suggests that PS-TKA achieves similar terminal flexion as the CR-TKA (125 – 130°) which remains less than a native knee (roughly 140°).
Advantages.
The PS-TKA is often easier to balance than CR-TKA because there are fewer ligaments to balance, and the kinematics are more consistent with the cam-post design.
Disadvantages.
Dislocation. The PS-TKA can dislocate, the cam jumps the post, if the flexion gap is too loose and the knee is placed under varus stress. Poly wear at the cam-post interface is a concern based on implant retrieval analysis. It appears that wear severity is highly dependent on ligament balancing (it is rarely an issue with a well balanced knee, but if the post is acting as a secondary stabilizer to coronal motion, it will wear out over time). More constrained implants, like the CCK discussed below, have increased contact between the cam-post because the role of this articulation is expended to providing medial-lateral stability and there is significantly more wear in these implants.
Patellar Clunk syndrome is associated with the PS-TKA because suprapatellar scar tissue can get caught within the cam as the knee goes into extension around 30-45° (the patella starts traveling proximally and the prominent scar tissue catches the lip). Treatment requires arthroscopic tissue removal.
PS-TKA requires additional bone removal from the distal femur - the box cut to make room for the cam.
A larger flexion gap because the PCL is removed, which requires compensatory larger distal femoral cut to balance the extension gap (the extra bone taken appears inconsequential, and does not appear to routinely create a patella baja, which requires about 8 mm in joint line elevation to cause symptoms).
Cruciate Retaining ("pcl retaining", CR-TKA)
The CR-TKA design utilizes the native PCL to prevent anterior translation of the femur during knee flexion, and therefore does not have the Cam-Post mechanism. The PCL is a knee stabilizer in flexion. Studies comparing CR-TKA with an intact PCL to the CR-TKA without the PCL showed significant decline in kinematics with the PCL absent, including decreased LFC posterior translation and paradoxical anterior translation of the MFC. This indicates that the PCL is critical to normal knee kinematics. One concern however, is that the soft tissue in an arthritic knee with significant deformity may not maintain function in the long term, and thus patients may be at risk for losing kinematic function over time if the PCL becomes attenuated or ruptures. Furthermore, some studies have suggested that the CR-TKA is less consistent in producing femoral rollback as compared to PS-TKA, regardless of perceived PCL functionality. The CR-TKA demonstrates paradoxical anterior translation of the femur, as well as minimal LFC rollback. One randomized control trial compared PS to CR TKA with regards to both kinematics and clinical outcome. It was demonstrated that despite more abnormal kinematics in the CR-TKA, both range of motion in weight bearing and non-weight bearing, and functional outcomes were equivalent up to 5 years later.
In the CR-TKA, the MFC has a larger radius of curvature as compared to the LFC to promote external rotation with knee flexion (this replicates the native knee where the MFC has a larger radius).
Advantages. The CR-TKA preserves femoral bone by not cutting away a central groove for the tibial post to track (“box cut”). The PCL also stabilizes the knee in flexion and may keep a tighter flexion gap when preserved.
Disadvantages. The CR-TKA is more challenging to balance because PCL tension enters the equation when balancing the flexion and extension gaps. The CR-TKA is also more challenging to balance with larger knee deformities (varus > 10°, valgus > 15°). And as mentioned before, PCL attenuation or rupture can lead to instability.
Hightly congruent liner ("Anterior stabilized")
The PCL is sacrificed yet the CR-TKA femur is used (there is no cam-post mechanism). Instead, a Highly-Congruent Liner (HCL) offers a highly-conforming articular geometry via a tibial polyethylene to control kinematics and give stability. In the native knee, the medial femoral condyle (MFC) and the lateral femoral condyle (LFC) do not move symmetrically, rather the larger MFC remains fairly immobile and acts as a pivot center, while the smaller LFC glides posteriorly during knee flexion causing external rotation and femoral rollback. This liner uses high articular congruence to guide this motion. The medial side concavity is spherical and holds the MFC in place while it rotates in flexion. The lateral side is more of a slot than a dish and this allows the LFC to glide posteriorly in flexion. The anterior lip of the poly is raised to prevent anterior translation of the femur.
Bicruciate Retaining (BCR-TKA)
The Bicruciate Retaining implant (BCR-TKA), similar to the unicondylar arthroplasty, is an Anatomic Design (the PS, CR, and HCL designs are all variations of the Mechanical Design). Anatomic design means recreating patients joint line (which is on average 3° of varus). It is more of a resurfacing procedure. Remember that knee motion is guided by soft tissue tension, muscle contraction and articular geometry. If the collateral ligaments and ACL and PCL ligaments are all being preserved (with no balancing) they will remain powerful drivers of knee kinematics. Therefore, the liner is completely flat to minimize articular congruency. This prevents a kinematic conflict: the ligaments are pulling the knee motion one way and the poly liner is guiding the knee motion another way. This was the underlying reason for failures of the early Anatomic Knee Designs.
It remains controversial whether cruciate preservation provides any proprioceptive advantage to patients. Histologic studies do show the presence of mechanoreceptors within the cruciate ligaments, however clinical studies fail to show significant differences in proprioception between the CR- and PS-TKA designs (one would expect preservation of the PCL would confer some proprioceptive advantage if these mechanoreceptors where significant).
The BCR-TKA is a more technically challenging procedure because more attention must be paid to soft tissue preservation. Furthermore, there is a stricter selection criteria because ligaments must be intact and knee deformity must be minimal because similar to UKA, there is little opportunity to adjust deformity.
References
1. Kim, Y.H., et al., Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am, 2009. 91(4): p. 753-60.
2. Chaudhary, R., L.A. Beaupre, and D.W. Johnston, Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am, 2008. 90(12): p. 2579-86.
3. Clark, C.R., et al., Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res, 2001(392): p. 208-12.
4. Maruyama, S., et al., Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty, 2004. 19(3): p. 349-53.
5. Peters, C.L., et al., Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop Relat Res, 2014. 472(1): p. 175-80.
3. Revision TKA Designs
The challenges of revision TKA is the need to address 1) Instability; 2) Bone Loss; and 3) recreate the joint line.
Ligament insufficiency is common in the revision setting and it causes instability. To compensate for lost ligament tension, the TKA implant must increase articular conformity, giving the articulation more constraint. Revision surgery often requires the device to offer varying degrees of coronal plane stability because the collaterals are compromised. This is where the constrained and hinged devices are important.
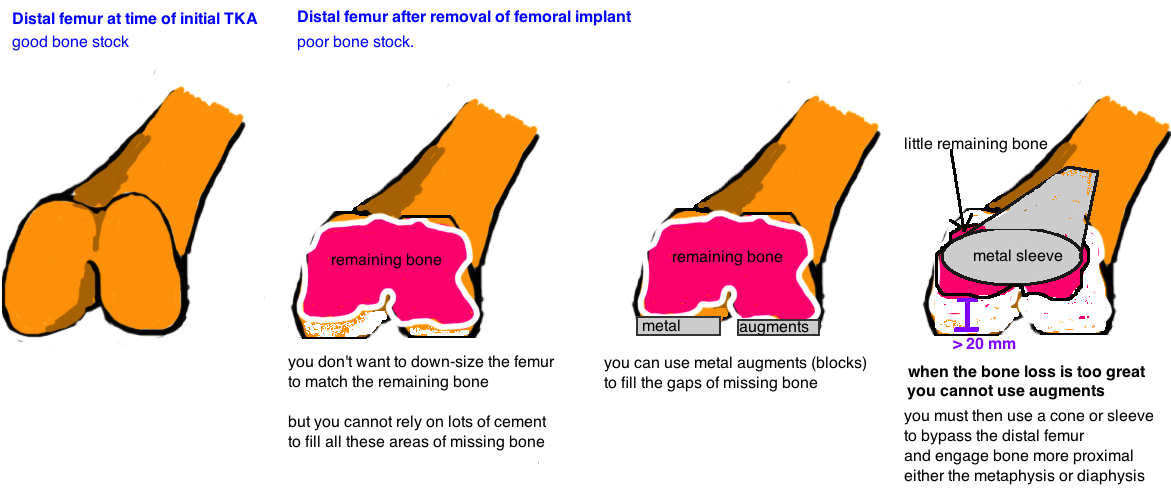
Bone loss occurs in varying degrees when primary implants are removed. Increased bone loss means less surface area of implant-bone interface for stress distribution. This increases the risk for aseptic loosening. Augments are available to replace the lost bone with metal and have proven effective for revision surgery. However, in cases of excessive bone loss, augments are not enough, and the entire distal femur or proximal tibia must be bypassed using cones or sleeves, which engage the metaphysis or diaphysis.
Instability
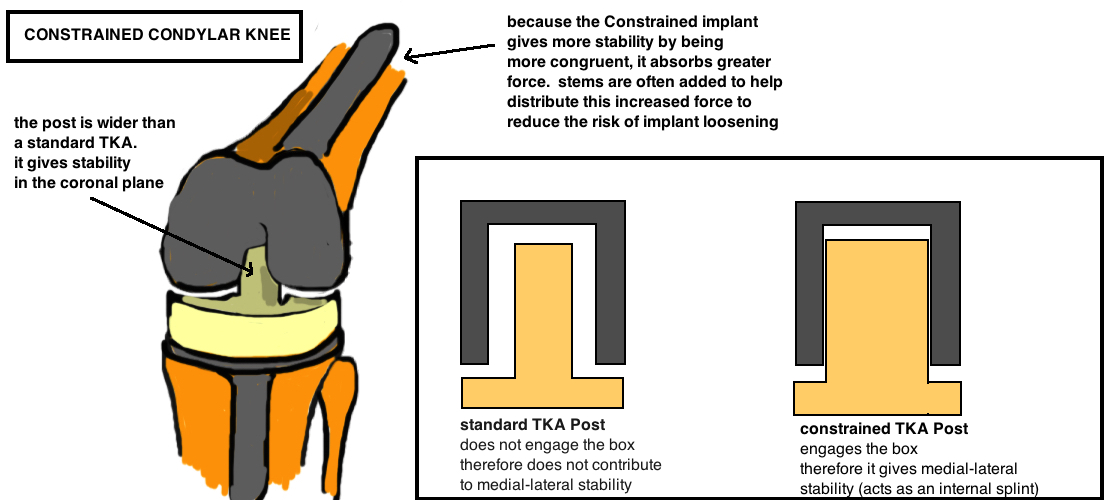
Constrained Implant. A constrained implant (ie CCK: constrained condylar knee) can be used when the soft tissue alone cannot provide enough stability to the knee. The constrained implant increases the width of the post on the poly to partially or fully engage the femoral implant box…thus increasing the articular congruency, and giving added stability in the coronal plane. This mechanism is an internal brace and reduces coronal motion to about 1° (or about 5° for partially constrained implants). Most CCK implants require a larger box cut to accommodate the wider post and thus implants are revised (although some designs just make the post wider and you can use the same femoral implant). Many surgeons add stem extensions to the CCK implant because its a more constrained implant and therefore it assumes greater stress during motion and more force is transmitted to the bone-cement interface which can lead to early loosening. Adding a stem to the implant will increase the surface area to distribute this increased stress, thus reducing risk of aseptic loosening.
.
Some implants are “partially constrained” meaning the constrained post is wider than a standard post but not completely congruent with the cam and therefore there is some wiggle room (maybe 5° as opposed to only 1° of coronal motion for the standard CCK) , and therefore, only the poly liner needs to be exchanged. The CCK offers stability in the coronal plane, but not in the saggital plane, therefore balanced flexion and extension gaps must be maintained. The CCK is sometimes used when the superficial MCL is damaged during surgery (ie released off the tibia) and it acts as an internal splint giving stability in the first 6 weeks until the soft tissues heal and then give further stability.
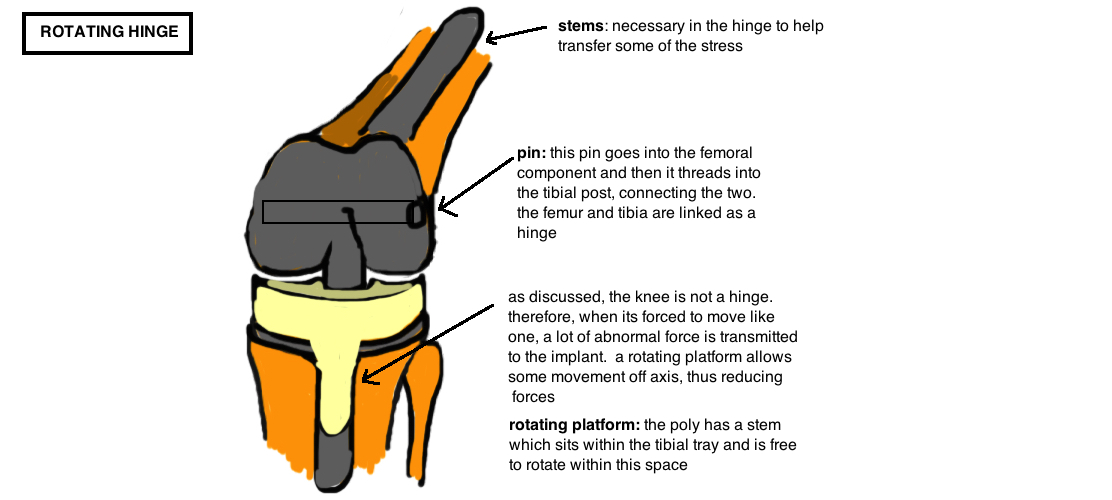
Hinge Implant. A hinge implant is used for complete ligament instability. If the MCL is completely missing, a CCK will experience excessive stress over time and will eventually fail due to poly wear or fracture. Therefore a hinge is recommended. Hinge is also recommended for global instability, anterior-posterior instability (hyperextension, ie Polio). Current hinge designs have a "rotating platform" to add some increased freedom at the articular surface (this takes away some of the stress translated to the implant-cement-bone interface...a fixed hinge transmits excessive force to the bone-cement interface and causes early failure). A PE liner rotates in a highly-polished tibial baseplate. Almost all hinges are rotating because of improved kinematics and reduced loosening (reduces the torque stress).
Additionally there is a segmental type hinge for large bone defects versus a condylar-type hinge for use in cases of good bone stock and deficient soft tissue, which is preferred because of better load distribution.
It is important to note that there is an increased risk of implant loosening when you increase the constraint. In a normal knee, stability is controlled by the muscles, ligaments and articular congruence and the stress across the knee are absorbed by all three things. However, as there is less and less soft tissue support for stability, then more and more of the stress will get transmitted to the implant because the more conforming articular geometry is absorbing the forces. This increased stress gets transmitted to the bone-cement interface. Over time, this increased stress can cause aseptic loosening. Many surgeons implant stems, which go up the femoral and tibial canals, to increase the surface area across which the stress is distributed. These stems are important to prevent increased loosening when there is increased constraint.
bone loss
Revision surgery often involves bone loss around the implant. Bone loss occurs when the primary implants are removed and varying amounts of native bone are lost in the process. Bone loss can occur due to osteolysis (from poly debris) or infection. Bone loss affects the stability of an implant because bone loss decreases the surface area of contact between the implant and bone. A decreased surface area increases the stress on bone-cement-implant interface and decreases long-term stability. Therefore, the fundamental goal of all techniques that addressing bone loss is to increase contact area between the bone and implant by identifying where there is stable bone and using various implants to achieve fixation in that region.
Cement alone can bridge a bone void that < 5 mm deep. A contained defect between 5 - 10 mm can be addressed if the cement is reinforced with metal screws thru the cement (referred to as "rebar").
Focal bone loss between 5 - 20 mm can also be addressed with augments. Augments can be added to femoral or tibial components at 5, 10, 15, or 20 mm sizes.
If the metaphyseal bone loss is too extensive for augments, Metaphyseal Sleeves or Cones are an option. These implants fill large metaphyseal defects with porous metal to allow ingrowth. If a sleeve/cone is used, then augments are not necessary because fixation is occurring proximally. The term "sleeve" and "cone" are often used interchangably because they perform the same function, yet there are subtle differences. A sleeve attaches to the stemmed implant to increase contact with bone, while a cone is a separate component, made of highly porous metal, that is placed into the metaphyseal bone defect and the stemmed implant is then cemented into the cone.
Lastly, there are times when the entire metaphysis (cortex and canellous bone) is completely absent. In these cases a distal femoral replacement, or proximal tibial replacement, is required because there is no bone for ingrowth.
Bone loss means less surface area for the bone-cement-implant interface, which means greater force is transmitted and this increases loosening. Stems engage the femoral/tibial canal and thus increase the surface area for better distribution of force in cases of significant bone loss. Stems are often added to implants with increased constraint (regardless of whether there are bone defects) because increased constraint causes increased force transmitted to the bone-cement-implant interface, and thus stems increase the surface area to accommodate the increased force .
UNICOMPARTMENTAL Knee Arthroplasty (UKA)
Unicompartmental arthroplasty is a partial knee replacement, it resurfaces either the medial (90%) or lateral(10%) compartment. UKA is becoming an increasingly popular procedure. In the 1990s, the high tibial osteotomy (HTO) was the gold standard procedure for treatment of unicompartmental arthritis, particularly in younger patients, while the UKA was avoided largely due to the stigma of high failure rate associated with the first generation of unis. At the Mayo clinic for example there were over 8,000 total knees performed in the 1990s and only 3 UKA, yet that number increased 50x between 2000 – 2003 while HTO procedures declined. In 2006, the medial compartment UKA was the procedure of choice in 11% and 29% of surgeons for a 45 year old male or female (respectively) with unicompartmental arthritis. The overall number nationally continues to rise in the 21st century, whereby roughly 10-15% of patients are indicated for this procedure. However indications remain controversial.
INDICATIONS
The initial indications were delineated by Kozin & Scott[1, 2]: isolated medial compartmental DJD (no lateral compartment arthritis, only mild patellofemoral arthritis on merchant view), no lateral joint line tenderness, intact ACL (look at the wear pattern on lateral x-ray of the knee: posterior tibial bone loss indicates disrupted ACL because the tibia has shifted anteriorly without the ACL restraint, exposing the posterior tibia to contact stresses from the distal femoral condyles); noninflammatory arthroplasty; weight under 82 kg; correctable varus deformity (< 5° deformity); over 60 years old; flex contracture <5°; range of motion > 90°.
This criteria served as the foundation for patient selection for decades even though there isn’t good data to support many of the specifics (and the criteria is surprisingly specific with regards to degrees, pounds, years, etc.) Recent studies have questioned many of the established thresholds. Scott et al. reevaluated his guidelines in a series of papers in CORR [3, 4], amending the age restriction by suggesting that the UKA is an alternative to the HTO in the younger population, increasing the weight restriction to 90 kg, and increasing the flexion contracture to <15 °, and < 10° varus or 5° valgus deformity.
The Nuffield Criteria similarly encourages modifications to the initial exclusion criteria, and suggests that patellofemoral arthritis, weight, age, and activity level should not be contraindications.
Expanded indications for UKA has been further supported by Berend, Lombardi et al [5]. They eliminated age, BMI, and activity level from the selection criteria without observing increased failure rates [6]. They report age (+/- 60) had no effect on outcomes; BMI >40 no effect on survivorship and patellofemoral arthrosis (as determined by Altman scoring system) similarly did not effect revision rates.
The necessity of ACL function is also controversial [7]. The ACL appears less important in fixed-bearing UKA compared to the Oxford mobile-bearing UKA, which requires more knee stability to prevent the mobile poly from dislocating (although studies show success with the Oxford UKA in the ACL-deficient knee as well). It is controversial whether the ACL is reliably intact in the arthritic knee. Studies suggest that 61% are intact in a knee with DJD [8], however, an aging knee becomes increasingly arthritic and the surrounding soft tissue envelop stiffens, and thus offers increased stability to the knee, reducing the role of the ACL. Furthermore, ACL function is probably not binary but rather its function diminishes with age as it becomes attenuated.
The exclusion of inflammatory arthritis is an important theoretic distinction in the progression of knee degeneration. Inflammatory arthritis creates a toxic environment to chondrocytes throughout the knee joint and therefore it is expected that all compartments of the knee will eventually develop arthritis. However, the natural history of primary osteoarthritis of the knee is less clear. If medial compartment arthritis is observed, will that arthritis progress to involve the patellofemoral joint and the lateral compartment? Is the medial compartment simply the first domino to fall, or can the progression be contained by addressing the medial compartment. Many argue that osteoarthritis can be contained. The conversion rate to TKA after a medial compartment UKA, due to arthritis progression, is less than 5% after 20 years. Why is this true, when tricompartmental arthritis is so common? One model for knee arthritis is a stepwise deterioration that begins with anterior-medial tibial wear (the focal contact point of the Medial Femoral Condyle, which moves very little during knee kinematics). The wear creates a varus deformity of the knee, which leads to increased stress on the ACL and meniscus, which leads to attenuation of these soft tissues and progression of arthritis to the posterior-medial tibia (the tibia subluxes anteriorly as the soft tissue restrains attenuate). As wear progresses, knee kinematics become deranged, patellofemoral wear worsens with abnormal tracking, and lateral compartment wear develops leading to tri-compartmental arthritis. Proponents of this theory believe the UKA is a great procedure because it stops disease progression, nips the arthritis at the bud, and preserves most of the native knee architecture[9].
DESIGN
We discussed the history of TKA above and highlighted to the two theories behind TKA design: anatomic and mechanical. The anatomy designs preserved the knee ligaments and allowed this soft tissue to control knee kinematics. However the more popular TKA design, the mechanical design, uses the surface geometry to primarily guide knee motion, and it sacrifices the cruciate ligaments, adjusts the tension of the collateral ligaments to achieve a mechically neutral knee that is amenable to being guided thru motion by the implant.
The UKA is primarily based on the anatomic design. The cruciate ligaments are preserved, the collateral ligament tension is not manipulated, and the implant is placed with the goal of “going with the flow”, it doesn’t want to get in the way of the knees natural motion. Even more specifically, the polyethylene bear surface cannot guide knee motion because it would create a “kinematic mismatch”, meaning the lateral compartment and the soft tissue envelop is guiding the knee along a very specific track while a UKA with a conforming poly would try guiding the knee along a different track and this would effectively prevent any smooth knee motion.
There are two design types for the UKA that create a stable implant without interfering with knee motion. Both have pros and cons. In both cases the femoral component is relatively the same. It’s the tibial side that varies.
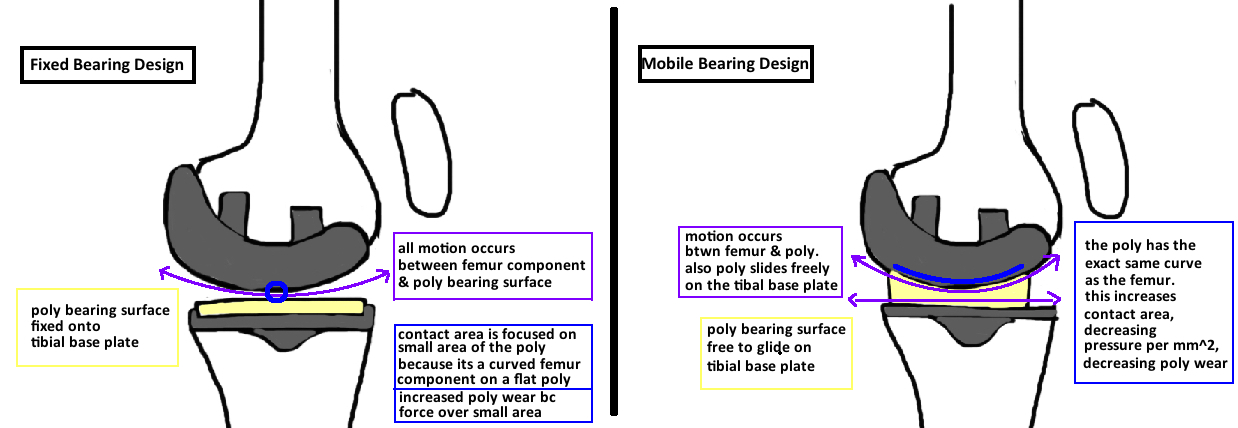
Fix-bearing design has a tibial segment where the polyethylene is fixed to the tibial base plate. This is essentially what you see in the TKA design. However, in the TKA design the poly is usually concave and this surface geometry guides some of the knee motion. However, this is avoided in UKA and therefore, the poly in a Fixed-bearing design is relatively flat so there is no guided motion from the articular geometry. The problem is that the femoral component is curved, and it is sitting on a flat poly, which focuses all of the force on a very small contact point. If pressure = force/area, and the contact area is small, then there is a lot of pressure on the poly and this can lead to accelerate wear. The concern above focused contact area is addressed in the mobile-bearing design.
Mobile-bearing design has a curved tibial poly that matches perfectly with the curve of the femoral component [10]. This conformity means that there is a large contact area and this diminishes the pressure on the poly and reduces wear. The problem is that we don’t want conformity between the femur and tibial because it will affect kinematics. This problem is avoided by allowing the poly to move freely on the tibial base plate. The rest of the knee will move the poly as needed as it remains conformed to the femoral component. This design is a great idea, and works great in reality, as long as the procedure is performed properly. The concern with this design is that the poly may be too free, and risks dislocating (which is a unique mode of failure for this mobile bearing design).
There is debate about which design is superior. There is evidence to support both sides. The mobile bearing design was developed by the Oxford Knee Group in England, and studies from that group demonstrate excellent survivorship (98% at 10 years, 92% at 15 years [11, 12]), while some studies based on registry data in other countries, Australia and Sweeden, show increased complications compared to the fixed-bearing design. Specifically the mobile UKA showed higher failure in first 3 years then a low steady state failure, which may be attributed to surgical technique. Together the results suggest that the Mobile Bearing design is more technically challenging and theres greater risk of failure for surgeons inexperienced with the procedure, however, if done properly, the outcomes are excellent. The Fixed Bearing design demonstrates excellent survivorship, although may not match that of the best mobile bearing studies. It appears to be more utilitarian, shorter learning curve, and good overall results.
The main advantage of the Mobile-bearing design was the increased contact surface on the poly that reduces poly wear. However, over the past decade, one could argue that a major paradigm shift has occurred in the material science of joint arthroplasty – the ultra-high molecular weight polyethylene (UHMWP). Increased cross-linking within the polyethylene has decreased wear. Other materials, such as the oxindium bearing surface (which is a hybrid ceramic material) also appears to have lower wear properties. In combination, its possible that wear will become so minor that the issue of poly wear will no long be a major limitation in the longevity of implants. This means that Fixed-bearing implants may offer equivalent survivorship to Mobile-bearing implants. It also means that a UKA is an increasingly good procedure for young patients who want to be very active with their implant.
Outcomes
The UKA has notable advantages over the TKA[13-15]: faster patient recovery, lower incidence of perioperative complications, higher patient satisfaction: better return to prior activity, better kinematics and feels more like a “normal knee”.
The surgery removes less bone and less soft tissue. Both are important variables in knee kinematics and studies demonstrate that a UKA better reapproximates normal knee motion. Recreation of knee kinematics is associated with improved patient satisfaction, as is lower pain scores and return to function. UKA appears to achieve higher patient satisfaction as compared to TKA (although these are patients with better knees at baseline so its comparing apples and oranges in some respects).
The UKA can be durable if done well and done in the properly selected patient.
The UKA are shown to be less durable than TKA but the difference is not dramatic. Metanalysis demonstrates UKA have 1.53%/year failure rates compared with 1.26%/year of TKA[16].
Age has a significant impact on survivorship. In patients under 55, that rate increases to 2.55%/year, 55-64 years old its 1.8%/year and over 65 its 1.3%/year. Although a study on UKA in patients under 60 demonstrate 90% survivorship at average of 11 years, with 90% satisfaction and return to sport [17].
Interestingly there is a higher number of UKA with excellent scores that still get revised. There is possibly an independent factor for the higher revision rate, because the TKA is always an option for postop pain, while a TKA does not have a good secondary option[10].
References
1. Kozinn, S.C., C. Marx, and R.D. Scott, Unicompartmental knee arthroplasty. A 4.5-6-year follow-up study with a metal-backed tibial component. J Arthroplasty, 1989. 4 Suppl: p. S1-10.
2. Kozinn, S.C. and R. Scott, Unicondylar knee arthroplasty. J Bone Joint Surg Am, 1989. 71(1): p. 145-50.
3. Deshmukh, R.V. and R.D. Scott, Unicompartmental knee arthroplasty: long-term results. Clin Orthop Relat Res, 2001(392): p. 272-8.
4. Scott, R.D., Unicondylar arthroplasty: redefining itself. Orthopedics, 2003. 26(9): p. 951-2.
5. Berend, K.R., A.V. Lombardi, Jr., and J.B. Adams, Obesity, young age, patellofemoral disease, and anterior knee pain: identifying the unicondylar arthroplasty patient in the United States. Orthopedics, 2007. 30(5 Suppl): p. 19-23.
6. Price, A.J., et al., Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg Br, 2005. 87(11): p. 1488-92.
7. Mancuso, F., et al., Medial unicompartmental knee arthroplasty in the ACL-deficient knee. J Orthop Traumatol, 2016. 17(3): p. 267-75.
8. Lee, G.C., et al., Evaluation of the anterior cruciate ligament integrity and degenerative arthritic patterns in patients undergoing total knee arthroplasty. J Arthroplasty, 2005. 20(1): p. 59-65.
9. Weale, A.E., et al., Does arthritis progress in the retained compartments after 'Oxford' medial unicompartmental arthroplasty? A clinical and radiological study with a minimum ten-year follow-up. J Bone Joint Surg Br, 1999. 81(5): p. 783-9.
10. Price, A.J., et al., A history of Oxford unicompartmental knee arthroplasty. Orthopedics, 2007. 30(5 Suppl): p. 7-10.
11. Murray, D.W., J.W. Goodfellow, and J.J. O'Connor, The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg Br, 1998. 80(6): p. 983-9.
12. Price, A.J., J.C. Waite, and U. Svard, Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res, 2005(435): p. 171-80.
13. Berend, K.R., J. George, and A.V. Lombardi, Jr., Unicompartmental knee arthroplasty to total knee arthroplasty conversion: assuring a primary outcome. Orthopedics, 2009. 32(9).
14. Lombardi, A.V., Jr., et al., Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res, 2009. 467(6): p. 1450-7.
15. Lygre, S.H., et al., Pain and function in patients after primary unicompartmental and total knee arthroplasty. J Bone Joint Surg Am, 2010. 92(18): p. 2890-7.
16. Labek, G., et al., Outcome and reproducibility of data concerning the Oxford unicompartmental knee arthroplasty: a structured literature review including arthroplasty registry data. Acta Orthop, 2011. 82(2): p. 131-5.
17. Felts, E., et al., Function and quality of life following medial unicompartmental knee arthroplasty in patients 60 years of age or younger. Orthop Traumatol Surg Res, 2010. 96(8): p. 861-7.