The goals of all TKA designs are to provide stability, longevity and normal kinematics.
The native knee relies on articular congruence, muscle tone, and soft tissue tension to guide motion.
As discussed in the History of TKA, the competing designs for TKA were anatomic vs. functional. The superior reproducibility of the “Functional Approach” lead it to become the gold standard. Within this group, the Cruciate-Sacrificing (CS-TKA) was first developed (the ICHL and the Total Condylar), with further development leading to the Posterior-Stabilized (PS-TKA) design (Insall-Burstein and its later derivations), and the Cruciate-Retaining design (CR-TKA, referring to preservation of the Posterior Cruciate Ligament). There are many randomized-control trials and meta-analyses comparing the PS and CR designs without demonstrating superiority in patient satisfaction, function, pain, or complications.
The standard primary TKA is comprised of a cemented Cobalt-Chrome femoral component, a polyethylene liner and a titanium tibial baseplate, and polyethylene patellar button (if the patella is resurfaced). The tibial component is not always a baseplate + liner, but can be a monoblock tibial poly (the poly liner is cemented directly onto the tibial bone without a metal baseplate).
Cobalt-Chrome is the material used for the femoral component because it wears slowly as a bearing surface, whereas titanium wears too fast to be utilized as bearing surface material. Titanium is however the preferred material for implants because it better matches the modulus of elasticity for bone and thus improves the time to implant loosening. Polyethylene actually has the closest match to a bones modulus of elasticity and this in part explains why a monoblock all-polyethylene tibia has the best longevity (in addition to avoiding backside wear).
The tibial component (poly liner + tibial base plate) starts at 9 mm thickness and can increase by 1 or 2 mm increments (depending on the system used). The more tibial bone resected, the larger the poly required. You are removing “x” millimeters of tibial bone, and replacing it with the same “x” millimeters of poly. The tibial base plate is about 2 mm thick and thickness doesn’t change. All additional thickness comes from the poly. The poly thickness is labeled as 9 mm etc but that measurement incorporates the 2 mm of tibial tray, and represents the thickest part of the poly. In reality, the concavity of the liner is thinner, maybe 5-6 mm, but if any thinner, the poly risks premature wear and fracture. That is why 9 mm is the target for smallest thickness.
Although the Oxford Uni system uses poly thickness of 3 or 4 mm. And there are no increased risk of poly damage, and if anything wear appears better.
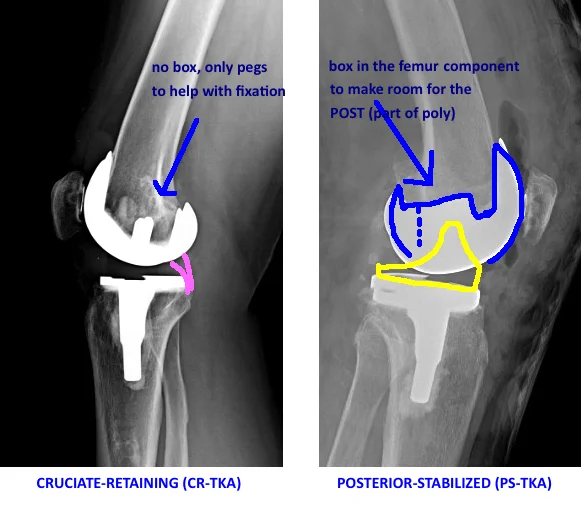
Two main designs of TKA
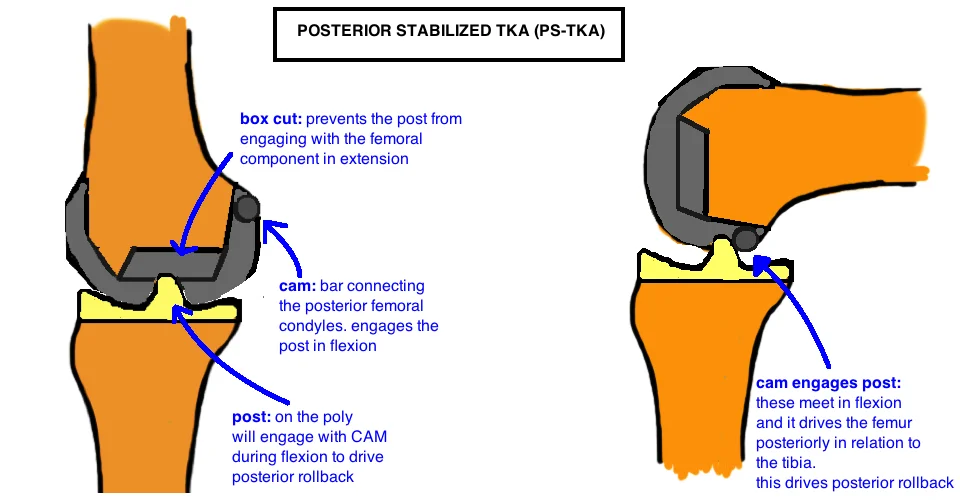
Posterior Stabilized (PS-TKA)
The Posterior-Stabilized TKA is designed with the goal of Mechanical Alignment. It relies on a tibial cut and femoral cuts that are perpendicular to the mechanical axis. The PS-TKA uses a Cam on the femur to engage to the back of the tibial Post (at 40 – 90° flexion) to push the femoro-tibial contact point posteriorly during knee flexion. This is “posterior rollback” and its essential for the knee to achieve deep flexion because terminal flexion occurs when the posterior femoral cortex impinges on the posterior tibial plateau (on the lateral side). By allowing the femur to rollback, it creates more offset before impingement occurs, enabling a deeper flexion. Historically, knee flexion in TKA was limited to 90° when there was no rollback (seen with the cruciate sacrificing TKA). The PS-TKA posterior rollback is only 80% of what is observed in the native knee. Yet in comparison to CR-TKA designs, it is generally considered to drive greater and more reliable rollback. Importantly this does not appear to influence functional outcome or even range of motion. Kinematic analysis suggests that PS-TKA achieves similar terminal flexion as the CR-TKA (125 – 130°) which remains less than a native knee (roughly 140°).
Advantages.
The PS-TKA is often easier to balance than CR-TKA because there are fewer ligaments to balance, and the kinematics are more consistent with the cam-post design.
Disadvantages.
Dislocation. The PS-TKA can dislocate, the cam jumps the post, if the flexion gap is too loose and the knee is placed under varus stress. Poly wear at the cam-post interface is a concern based on implant retrieval analysis. It appears that wear severity is highly dependent on ligament balancing (it is rarely an issue with a well balanced knee, but if the post is acting as a secondary stabilizer to coronal motion, it will wear out over time). More constrained implants, like the CCK discussed below, have increased contact between the cam-post because the role of this articulation is expended to providing medial-lateral stability and there is significantly more wear in these implants.
Patellar Clunk syndrome is associated with the PS-TKA because suprapatellar scar tissue can get caught within the cam as the knee goes into extension around 30-45° (the patella starts traveling proximally and the prominent scar tissue catches the lip). Treatment requires arthroscopic tissue removal.
PS-TKA requires additional bone removal from the distal femur - the box cut to make room for the cam.
A larger flexion gap because the PCL is removed, which requires compensatory larger distal femoral cut to balance the extension gap (the extra bone taken appears inconsequential, and does not appear to routinely create a patella baja, which requires about 8 mm in joint line elevation to cause symptoms).
Cruciate Retaining ("pcl retaining", CR-TKA)
The CR-TKA design utilizes the native PCL to prevent anterior translation of the femur during knee flexion, and therefore does not have the Cam-Post mechanism. The PCL is a knee stabilizer in flexion. Studies comparing CR-TKA with an intact PCL to the CR-TKA without the PCL showed significant decline in kinematics with the PCL absent, including decreased LFC posterior translation and paradoxical anterior translation of the MFC. This indicates that the PCL is critical to normal knee kinematics. One concern however, is that the soft tissue in an arthritic knee with significant deformity may not maintain function in the long term, and thus patients may be at risk for losing kinematic function over time if the PCL becomes attenuated or ruptures. Furthermore, some studies have suggested that the CR-TKA is less consistent in producing femoral rollback as compared to PS-TKA, regardless of perceived PCL functionality. The CR-TKA demonstrates paradoxical anterior translation of the femur, as well as minimal LFC rollback. One randomized control trial compared PS to CR TKA with regards to both kinematics and clinical outcome. It was demonstrated that despite more abnormal kinematics in the CR-TKA, both range of motion in weight bearing and non-weight bearing, and functional outcomes were equivalent up to 5 years later.
In the CR-TKA, the MFC has a larger radius of curvature as compared to the LFC to promote external rotation with knee flexion (this replicates the native knee where the MFC has a larger radius).
Advantages. The CR-TKA preserves femoral bone by not cutting away a central groove for the tibial post to track (“box cut”). The PCL also stabilizes the knee in flexion and may keep a tighter flexion gap when preserved.
Disadvantages. The CR-TKA is more challenging to balance because PCL tension enters the equation when balancing the flexion and extension gaps. The CR-TKA is also more challenging to balance with larger knee deformities (varus > 10°, valgus > 15°). And as mentioned before, PCL attenuation or rupture can lead to instability.
Hightly congruent liner ("Anterior stabilized")
There are many names for this system - anterior stabilized, highly congruent, medial congruent, medial pivot, etc.
The PCL can be sacrificed, but can also be preserved. Regardless the CR-TKA femur is used (there is no cam-post mechanism). The Anterior-Posterior stability is conferred by a Highly-Congruent Liner (HCL), which is a highly-conforming articular geometry within the medial compartment of the tibial polyethylene liner which will control kinematics and give stability.
In the native knee, the medial femoral condyle (MFC) and the lateral femoral condyle (LFC) do not move symmetrically, rather the larger MFC remains fairly immobile and acts as a pivot center, while the smaller LFC glides posteriorly during knee flexion causing external rotation and femoral rollback. This liner uses high articular congruence to guide this motion. The medial side concavity is spherical and holds the MFC in place while it rotates in flexion. The lateral side is more of a slot than a dish and this allows the LFC to glide posteriorly in flexion. The anterior lip of the poly is raised to prevent anterior translation of the femur.
Bicruciate Retaining (BCR-TKA)
The Bicruciate Retaining implant (BCR-TKA), similar to the unicondylar arthroplasty, is an Anatomic Design (the PS, CR, and HCL designs are all variations of the Mechanical Design). Anatomic design means recreating patients joint line (which is on average 3° of varus). It is more of a resurfacing procedure. Remember that knee motion is guided by soft tissue tension, muscle contraction and articular geometry. If the collateral ligaments and ACL and PCL ligaments are all being preserved (with no balancing) they will remain powerful drivers of knee kinematics. Therefore, the liner is completely flat to minimize articular congruency. This prevents a kinematic conflict: the ligaments are pulling the knee motion one way and the poly liner is guiding the knee motion another way. This was the underlying reason for failures of the early Anatomic Knee Designs.
It remains controversial whether cruciate preservation provides any proprioceptive advantage to patients. Histologic studies do show the presence of mechanoreceptors within the cruciate ligaments, however clinical studies fail to show significant differences in proprioception between the CR- and PS-TKA designs (one would expect preservation of the PCL would confer some proprioceptive advantage if these mechanoreceptors where significant).
The BCR-TKA is a more technically challenging procedure because more attention must be paid to soft tissue preservation. Furthermore, there is a stricter selection criteria because ligaments must be intact and knee deformity must be minimal because similar to UKA, there is little opportunity to adjust deformity.
REFERENCES
1. Kim, Y.H., et al., Functional outcome and range of motion of high-flexion posterior cruciate-retaining and high-flexion posterior cruciate-substituting total knee prostheses. A prospective, randomized study. J Bone Joint Surg Am, 2009. 91(4): p. 753-60.
2. Chaudhary, R., L.A. Beaupre, and D.W. Johnston, Knee range of motion during the first two years after use of posterior cruciate-stabilizing or posterior cruciate-retaining total knee prostheses. A randomized clinical trial. J Bone Joint Surg Am, 2008. 90(12): p. 2579-86.
3. Clark, C.R., et al., Posterior-stabilized and cruciate-retaining total knee replacement: a randomized study. Clin Orthop Relat Res, 2001(392): p. 208-12.
4. Maruyama, S., et al., Functional comparison of posterior cruciate-retaining versus posterior stabilized total knee arthroplasty. J Arthroplasty, 2004. 19(3): p. 349-53.
5. Peters, C.L., et al., Comparison of total knee arthroplasty with highly congruent anterior-stabilized bearings versus a cruciate-retaining design. Clin Orthop Relat Res, 2014. 472(1): p. 175-80.