Over 50,000 revision TKA are performed in the USA every year and this number is growing as patients are living longer. Its projected to rise 600% by 2030. The most common reasons for revision include aseptic loosening (28%), septic loosening (14%), pain without known etiology (9%).
Selection of the Revision TKA will be affected by 1) Instability, 2) Bone Loss.
Instability
Ligament insufficiency is common in the revision setting and it causes instability. The TKA implant must increase articular congruity to give the implant more constraint to compensate for lost ligament tension. Revision implants offer varying degrees of coronal plane stability by increasing the congruency of the tibial post and the femoral box. This is where the constrained and hinged devices are important.
Constrained Implant.
A constrained implant (ie CCK: "constrained condylar knee") can be used when the soft tissue alone cannot provide enough stability to the knee. The constrained implant increases the width of the post on the poly to partially or fully engage the femoral implant box…thus increasing the articular congruency, and giving added stability in the coronal plane. This mechanism is an internal brace and reduces coronal motion to about 1° (or about 5° for partially constrained implants). Many constrained implants require a larger box cut to accommodate the taller and wider post and thus implants are revised (although some designs just make the post only slightly larger and don't require a different size femoral box, thus allowing you to keep the same femoral implant, if desired). Many surgeons add stem extensions to the constrained implant, because a more constrained implant assumes greater stress during motion and more force is transmitted to the bone-cement interface which risks early loosening. Adding a stem to the implant will increase the bone-cement surface area to distribute this increased stress, thus reducing risk of aseptic loosening.
Some implants are “partially constrained” meaning the constrained post is wider than a standard post but not completely congruent with the cam and therefore there is some wiggle room (maybe 5° as opposed to only 1° of coronal motion for the standard CCK) , and therefore, only the poly liner needs to be exchanged. The CCK offers stability in the coronal plane, but not in the saggital plane, therefore balanced flexion and extension gaps must be maintained. The CCK is sometimes used when the superficial MCL is damaged during surgery (ie released off the tibia) and it acts as an internal splint giving stability in the first 6 weeks until the soft tissues heal and then give further stability.
Hinge Implant. A hinge implant is used for complete ligament instability. If the MCL is completely missing, a CCK will experience excessive stress over time and will eventually fail due to poly wear or fracture. Therefore a hinge is recommended. Hinge is also recommended for global instability, anterior-posterior instability (hyperextension, ie Polio). Current hinge designs have a "rotating platform" to add some increased freedom at the articular surface (this takes away some of the stress translated to the implant-cement-bone interface...a fixed hinge transmits excessive force to the bone-cement interface and causes early failure). A PE liner rotates in a highly-polished tibial baseplate. Almost all hinges are rotating because of improved kinematics and reduced loosening (reduces the torque stress).
Additionally there is a segmental type hinge for large bone defects versus a condylar-type hinge for use in cases of good bone stock and deficient soft tissue, which is preferred because of better load distribution.
It is important to note that there is an increased risk of implant loosening when you increase the constraint. In a normal knee, stability is controlled by the muscles, ligaments and articular congruence and the stress across the knee are absorbed by all three things. However, as there is less and less soft tissue support for stability, then more and more of the stress will get transmitted to the implant because the more conforming articular geometry is absorbing the forces. This increased stress gets transmitted to the bone-cement interface. Over time, this increased stress can cause aseptic loosening. Many surgeons implant stems, which go up the femoral and tibial canals, to increase the surface area across which the stress is distributed. These stems are important to prevent increased loosening when there is increased constraint.
bone loss
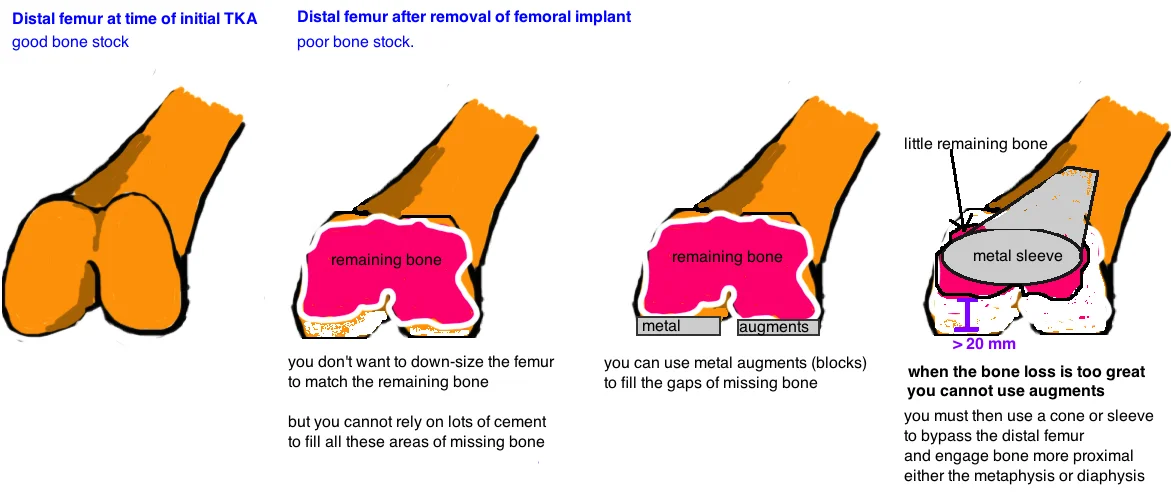
Revision surgery often involves bone loss around the implant. Bone loss occurs when the primary implants are removed and varying amounts of native bone are lost in the process. Bone loss can occur due to osteolysis or infection or from bone attached to the implants that are removed.
Bone loss affects the stability of an implant because it decreases the surface area of contact between the implant and bone. Decreased surface area increases the stress on bone-cement-implant interface and decreases long-term stability. Therefore, the fundamental goal of all techniques that address bone loss is to increase contact area between good bone and implant.
Cement alone can bridge a bone void that < 5 mm deep. A contained defect between 5 - 10 mm can be addressed if the cement is reinforced with metal screws thru the cement (referred to as "rebar").
Focal bone loss between 5 - 20 mm can also be addressed with augments. Augments can be added to femoral or tibial components at 5, 10, 15, or 20 mm sizes.
If the metaphyseal cortex is intact but the cancellous bone loss is too extensive for augments, Metaphyseal Sleeves or Cones are an option. These implants fill large metaphyseal defects with porous metal to allow ingrowth. If a sleeve/cone is used, then augments are not necessary because fixation is occurring proximally. The term "sleeve" and "cone" are often used interchangably because they perform the same function, yet there are subtle differences. A sleeve attaches to the stemmed implant, while a cone is a separate component, made of highly porous metal, that is placed into the metaphyseal bone defect and the stemmed implant is then cemented into the cone.
Lastly, there are times when the entire metaphysis (cortex and canellous bone) is absent. In these cases a distal femoral replacement, or proximal tibial replacement, is required because there is no bone for ingrowth.
Stems. Bone loss means less surface area for the bone-cement-implant interface, which means greater force is transmitted and this increases loosening. Stems engage the femoral/tibial canal and thus increase the surface area for better distribution of force in cases of significant bone loss. Stems are often added to implants with increased constraint (regardless of whether there are bone defects) because increased constraint causes increased force transmitted to the bone-cement-implant interface, and thus stems increase the surface area to accommodate the increased force .
Technique of Revision TKA
Approach. Careful evaluation of skin quality and prior incisions. Principles of skin blood supply should be maintained. Arthrotomy may require a more extensile exposure if knee is stiff. The Quad Snip or Tibial Tubercle Osteotomy effective mobilize the extensor mechanism to expose the joint.
Mobilization. The knee in extension allows for evaluation of the medial and lateral gutters, which often require fibrous debulking to give sufficient flexion and extension (be careful not to damage the collateral ligaments). Trying to forcefully flex the knee puts the patellar tendon at risk. Additionally, try to avoid patellar eversion due to risk of tendon avulsion (if this is a significant concern, place a pin into the medial side of the tendon as a piton).
Implant removal. A good preop plan is necessary to predict difficulties. Know the implants being removed. Predict if implants are fixed or loose, but have removal tools available regardless. There is a sequence of removal that optimizes visualization.
1. Remove poly. Use narrow curved osteotome to disengage from the tray.
2. Remove femoral component. Removing implants without removing too much bone is the biggest challenge. Aim the osteotome at the the implant-cement (not cement-bone) interface. If already loose, place impactor over the anterior flange.
3. Remove tibial component. Must be able to hyperflex knee to clear the posterior-lateral tibial condyle.
Re-implantation. Evaluating bone loss and choosing implant that restores stability. Cones or sleeves are used to compensate for metaphyseal bone loss. Augments along the distal femur or posterior femur (sizes 5, 10, 15 mm) can be used on the femoral implant to build up the areas of bone loss (cement cannot be used reliably to fill bone defects > 5 mm. Stems should be used if augments or cones are required. Constrained implants or hinged implants may be needed if there is ligament insufficiency. Restoring the joint line is key to obtaining good postoperative motion.