Most cases of AVN occur in 3-5th decade of life and are idiopathic, although its also associated with: trauma (particularly native hip dislocation – occurring in 10-25% of cases, and displaced femoral neck fractures – occurring in 15-50% of cases), alcoholism, steroid use (uncommon overall, and only 2% of patients with liver transplants, exposed to continuous , high level steroid developed symptomatic avn [16]), sickle cell disease and other coagulopathies, and autoimmune disease. AVN is the underlying etio for 5-12% of THA cases.
DIAGNOSIS.
Secondary AVN occurs bilaterally in 80% of cases to be sure to examine both hips.
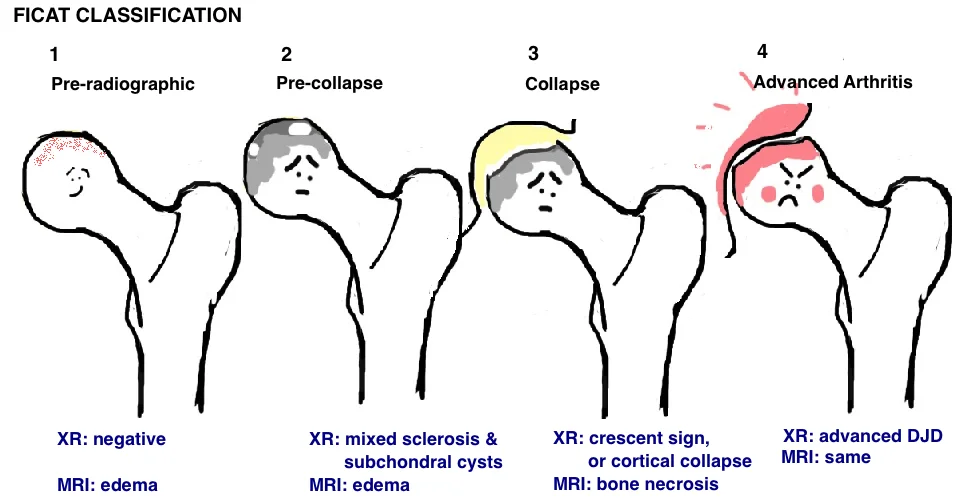
Hip AVN is diagnosed and staged with hip AP and frog-leg lateral, and MRI studies. Early stages of AVN will only appear as edema on MRI. Progression will then be seen on Hip XR as cystic and sclerotic changes in the femoral head, the “Crescent Sign” will develop (subchondral lucency which represents delamination of the cartilage, and is a poor prognostic sign), and this will be followed by femoral head collapse and progressive degeneration of the hip joint (involving both the femoral head and acetabulum). MRI is 99% sensitive and specific for AVN of the hip. AVN is typically progressive, yet there are
PROGNOSTIC FACTORS FOR FEMORAL HEAD COLLAPSE.
% involvement of the femoral head (proportion of cross-sectional involvement) [21].
-if <30%: low risk collapse (at 5 yrs): 5%
-if 30 – 50%: moderate risk collapse: 46%
-if >50%: high risk collapse: 83%
Combined Angle of Necrosis in the Mid-saggital + Mid-coronal cuts on MRI (this is the Modified Kerboul method). The implications on collapse was studied by Ha et al[17].
- if < 190° combined angle = low risk of collapse
-if 190 – 240° combined angle = moderate risk (50%)
-if >240° combined angle = high risk of collapse (near 100%)
Location. AVN in the weight bearing area has the greatest impact on collapse. One study found that 8/9 hips did not collapse when necrosis was < 2/3 of weight bearing area[18].
Edema. When the initial MRI (at the early stage of AVN) demonstrates significant edema in the proximal femur, there is a higher risk of progression and persistent symptoms[19].
Pain. Proceeds collapse.
TREATMENT.
There is no proven best method of joint preservation with AVN, however, a number of approaches have emerged. There is a lot of conflicting evidence for each treatment modality, and much of this may stem from our incomplete knowledge of the underlying cause of AVN and therefore, we are lumping together dissimilar patients for treatments.
Ficat Classification utilizes the findings on XR and MRI to stage the severity of AVN, and guide treatment (see table).
Non-surgical. It appears that even small lesions prove problematic over time, although the results are variable (suggesting that underlying factors determining outcome have not been fully identified). One study looking at small lesions (<10% femoral head volume) with over 10 years follow up, showed 88% symptomatic and 73% demonstrated some collapse [20]. A separate study showed only 5% collapse at 5 years in small lesions (<30% femoral head), while the overall rate of collapse (all comers) was 59% [21]. A systemic review looking at patients around 5 years follow up indicated that 66% required surgical intervention and 72% showed progression on X-ray[22]. Therefore the concensus is that non-surgical treatment (ie nonweight bearing) should have a very limited role in the treatment of AVN.
Core decompression. The goal is to reduce pressure within the femoral head and restore vascularity to stimulate healing. The key to core decompression is performing the procedure pre-collapse. Core decompression can be performed alone, or in conjunction with bone graft, nonvascularized fibular graft of vascularized fibular graft (VFG). One study found lower rates of THA at a minimum of 2 years (only 42% with lesions >30% of femoral head) [23]. Another demonstrated that only 30% of patients required a second procedure, and 63% had good outcomes on XR[22]. Other studies found no difference in collapse rate in those treated with core decompression[17]. Supplementing core decompression with bone marrow aspirate[24] or BMP [25] shows some potential for slowing progression.
Vascularized Fibular Graft (VFG). Appears to have the biggest impact on reversing disease progression. Studies report 86% survival of precollapse hips at 7 years (vs. 30% with nonvascularized graft) [26], although it appears less successful in post-collapse hips with 44% showing progressive changes by 5 years[27].
Bisphosphonates (alendronate). Pharmacologics have been studied for treating early (pre-collapse) AVN. The results are mixed, with one study showing low incidence of collapse, and another study showing no impact on collapse or need for THA.
THA. Outcomes of THA for AVN were historically associated with higher dislocation rates (due to better preop motion) and higher revision rates (younger, more demanding patients) [28]. However, recent studies suggest a low revision rate, and comparable to THA for osteoarthritis[29]. Hip resurfacing can also be considered in the younger patients, but its recommended only when AVN <50% of the femoral head, and standard complications like MoM and femoral neck fracture must be considered.
REFERENCES
16. Lieberman, J.R., A.A. Scaduto, and E. Wellmeyer, Symptomatic osteonecrosis of the hip after orthotopic liver transplantation. J Arthroplasty, 2000. 15(6): p. 767-71.
17. Ha, Y.C., et al., Prediction of collapse in femoral head osteonecrosis: a modified Kerboul method with use of magnetic resonance images. J Bone Joint Surg Am, 2006. 88 Suppl 3: p. 35-40.
18. Nishii, T., et al., Progression and cessation of collapse in osteonecrosis of the femoral head. Clin Orthop Relat Res, 2002(400): p. 149-57.
19. Ito, H., T. Matsuno, and A. Minami, Relationship between bone marrow edema and development of symptoms in patients with osteonecrosis of the femoral head. AJR Am J Roentgenol, 2006. 186(6): p. 1761-70.
20. Hernigou, P., et al., Fate of very small asymptomatic stage-I osteonecrotic lesions of the hip. J Bone Joint Surg Am, 2004. 86-A(12): p. 2589-93.
21. Nam, K.W., et al., Fate of untreated asymptomatic osteonecrosis of the femoral head. J Bone Joint Surg Am, 2008. 90(3): p. 477-84.
22. Marker, D.R., et al., Do modern techniques improve core decompression outcomes for hip osteonecrosis? Clin Orthop Relat Res, 2008. 466(5): p. 1093-103.
23. Israelite, C., et al., Bilateral core decompression for osteonecrosis of the femoral head. Clin Orthop Relat Res, 2005. 441: p. 285-90.
24. Hernigou, P. and F. Beaujean, Treatment of osteonecrosis with autologous bone marrow grafting. Clin Orthop Relat Res, 2002(405): p. 14-23.
25. Lieberman, J.R., A. Conduah, and M.R. Urist, Treatment of osteonecrosis of the femoral head with core decompression and human bone morphogenetic protein. Clin Orthop Relat Res, 2004(429): p. 139-45.
26. Plakseychuk, A.Y., et al., Vascularized compared with nonvascularized fibular grafting for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am, 2003. 85-A(4): p. 589-96.
27. Soucacos, P.N., et al., Treatment of avascular necrosis of the femoral head with vascularized fibular transplant. Clin Orthop Relat Res, 2001(386): p. 120-30.
28. Ortiguera, C.J., I.T. Pulliam, and M.E. Cabanela, Total hip arthroplasty for osteonecrosis: matched-pair analysis of 188 hips with long-term follow-up. J Arthroplasty, 1999. 14(1): p. 21-8.
29. Kim, S.M., et al., Cementless modular total hip arthroplasty in patients younger than fifty with femoral head osteonecrosis: minimum fifteen-year follow-up. J Arthroplasty, 2013. 28(3): p. 504-9.