Gradual but progressive cartilage wear is the most common indication for THA in people over 55 yo. Osteoarthritis is a term used in place of idiopathic arthritis, suggesting no underlying cause for the cartilage degeneration.
Yet many argue that any hip with arthritis is abnormal...in either morphology or underlying genetics and doctors have just not yet found the cause – the absence of evidence is not evidence of absence. But why is all arthritis abnormal? Because all forms of arthritis possess an inflammatory component that is absent from normal aging. Lets get technical for a moment by looking at the molecular level.
Cartilage at the molecular level. Cartilage is best understood as meshwork that resists compressive pressure via the regulation of water. Proteoglycans attract water while collagen forms a matrix that gives a surrounding structure.
Proteoglycans look like a tree with a trunk-branches-leaves. The trunk is the hyaluronic acid backbone, the braches are a protein called aggrecan, and the leaves are GAGs (chondroitin and keratin sulfate) which possess a highly negative charge (from the sulfate compound) that generates an osmotic gradient to pull in water. Proteoglycans are highly concentrated in the “deep layer” of cartilage, like a magnet at the core.
Our body use water as a shock absorber, to resist compressive loads, but the uncontrolled influx of water just creates swelling, which is not functionally useful. Therefore, our body has created a scaffolding around the proteoglycans, made of type 2 collagen and reinforced with type 9 collagen, to limit the swelling and create “fluid pressurization”. During joint loading, the big net of collagen holds the proteoglycans in place, and by preventing deformity, it increases pressure within the cartilage, and this pushes water out of the cartilage scaffold and into the joint space, where it lubricates. When the joint is subsequently unloaded, the negative charges of the GAGs repel, recreating the osmotic pressure, which pulls water and nutrients back into the cartilage. This system is called - “exchangeable water”.
Normal aging. Over time cartilage breaks down as the body loses its anabolic response to TGF-ß . Fewer proteoglycans and GAGs are produced, which diminishes the negative charge that attracts water, so the cartilage starts drying out. Collagen 9 decreases, so the underlying structure becomes more brittle, and cartilage end products slowly accumulate which turns the cartilage yellow. The body increases cartilage cross-linking via the molecule “decorin”, which increases the stiffness (read: modulus of elasticity), but further increases its brittleness and decreases its overall strength (just like highly-crosslinked PE!).
Osteoarthritis. A pro-inflammatory state forms within the joint that increases the expression of degenerative enzymes (cytokines, and proteases) that directly damage the components of cartilage. IL-1 stimulates matrix metalloproteases (degrades collagen), ADAMTS proteases, and stromelysin (degrades aggrecans). Therefore, the early phase of arthritis sees generalized cartilage injury. A drop in proteoglycans and aggrecans leads to free-floating GAGs. Collagen breakdown reduces control over the osmotic gradient, and there is more permeability and swelling, which decreases stiffness and strength of the matrix, further increasing its risk for breakdown. There is an increase in DAMPS (cartilage breakdown products), which include Hyaluronan, Fibronectant, and Collagen X.
The middle phase of arthritis is a response to this injury. Chondrocytes try to compensate by proliferating and increasing both anabolic activity (forming ECM) and catabolic activity (removing debris).
The late phase of arthritis, the chondrocytes are burnt out, and theres reduced chondrocyte activity, reduced anabolic activity, reduced water, and reduced compressive modulus.
What is the stimulus for Osteoarthritis?
Recent trends toward structural etiology for hip degeneration is currently in vogue (see DDH and FAI). Studies are being performed to better understand the role of obesity, genetics, and abnormal morphology. Obesity may accelerate the rate of hip degeneration. Biomechanically it increases forces across the hip. If climbing stairs creates a force 5x body weight, then body weight exerts a significant effect on the hip (just losing 10 lbs decreases the force on the hip by 50 lbs while stair climbing). Genetics of osteoarthritis are poorly understood.
▪ On Exam, progressive arthritis causes the hip to be flexed, externally rotated (near all internal rotation is lost), and adducted (develop abduction contracture). These changes lead to apparent limb shortening (which can lead to percieved limb lengthening after THA).
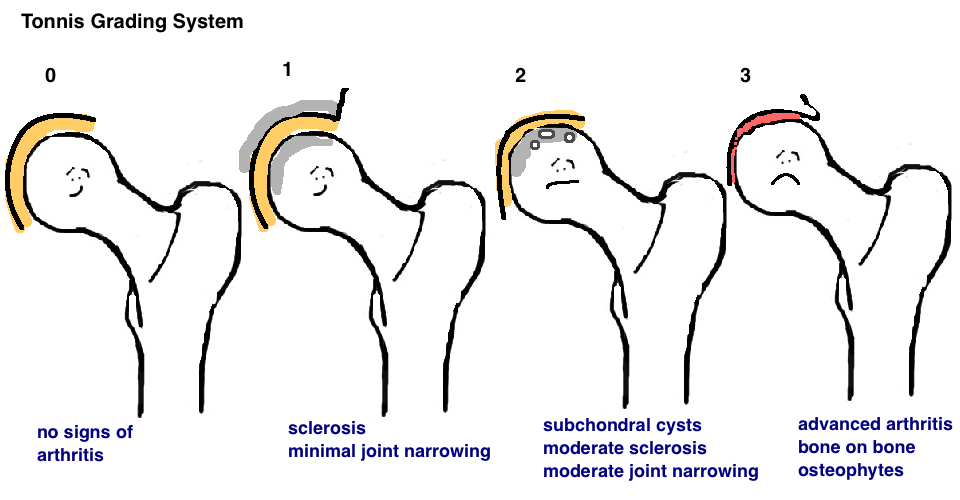
▪On X-Ray, hip osteoarthritis is described with reference to "sclerosis" "subchondral cysts" "joint space narrowing" and any morphological changes to the joint, such as femoral head collapse (as seen in AVN, below)) or acetabular dysplasia (as seen in DDH, below). The Tönnis Grading System can be used to describe hip osteoarthritis, although its infrequently used in practice.