-In 1912: The first surgical procedures to treat hip osteoarthritis were interposition grafts. Sir Robert Jones placed gold foil within the joint space, others used native soft tissue like fascia lata or synovial tissue.
-In 1923: Dr. Marius “Mads” Smith-Petersen pioneered the Mould-Arthroplasty procedure in Boston. The technique placed a glass mold over the femoral head to stimulate fibrocartilage metaplasia and form a smooth articular surface (the idea came to him after discovering a smooth synovial membrane surrounding a glass shard pulled out of a patient’s back). Not surprisingly, the glass broke after a few months, however, the very-short-term results were positive, and thus more durable materials were utilized (first pyrex, and then Vitallium…a metal alloy, see below). [23]. It was the first attempt at a surgical procedure to restore the joint instead interposing tissue.
-In 1932: Dr. Charles Venable and Dr. Walter Stuck, after studying for many years the effects of various metals on bone, discovered an alloy they called Vitallium [(cobalt (65%) - chromium (30%) - molibdenum (5%)] and one of the first metals found to be completely electrically inert within body fluid, showing no signs of corrosion or pathologic changes to bone). The material was first used to make plates and screws for fracture fixation, as was later adapted for femoral head prostheses.
-In 1937: Smith-Petersen (first heard of this vitallium from his dentist who was using it for fillings, not from his orthopaedic colleagues) created the vitallium cup arthroplasty, which molded around the femoral head articular surface, and similarly struggled early fragmentation.
-In 1939: Dr. Venable worked with Dr. Harold Bohlman to design a Vitallium implant that replaced the femoral head (rather than cover it), similar to today’s hemiarthroplasty (it attached the vitallium femoral head to a small intramedullary nail). Dr. Venable was the first to perform a hemiarthroplasty for a hip fracture.
Around the same time, the Judet Bros (Paris, France) created a heat-cured acrylic femoral head for a similar hemiarthroplasty design that experienced high rates of early failure due to rapid wear and severe tissue reaction (considered the first cases of osteolysis).
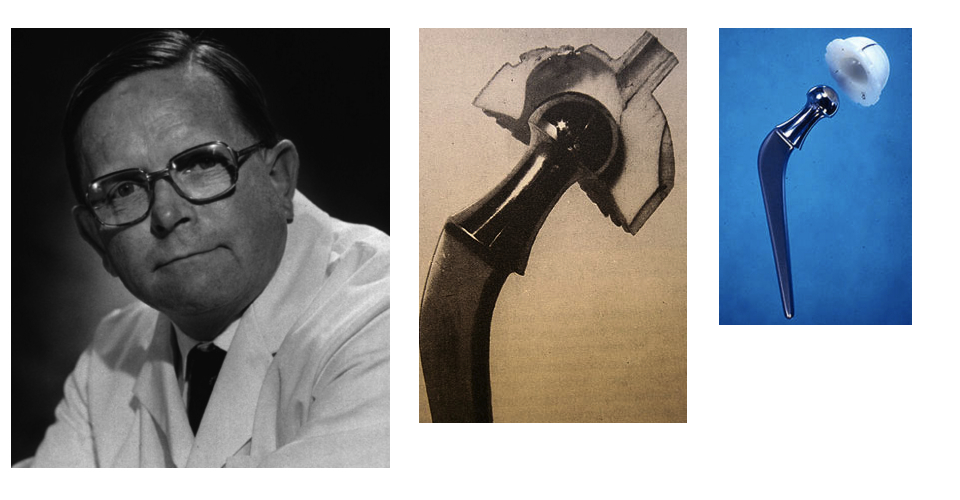
-In 1940s: Dr. Austin Moore (who was a surgeon at a psychiatric hospital in Maryland) worked further with Dr. Bohlman to improve the hemiarthroplasty design, and introduced the process of fixing the femoral head to a stem that would fit the proximal femur medullary canal
-In 1952: Dr. Moore and Bohlman introduced the stem that would allow for bone ingrowth (work was done at Austenal Labs which became Howmedica Inc. which became Stryker Corp.), and these produces were widely distributed, became legendary and are still used for some elderly femoral neck fractures.
-In 1950: Dr. Fredrick Thompson created a Vitallium prosthesis, similar to the Moore type prosthesis, which used cement to fix the stem to the femur. The prostheses developed by Dr. Moore and Thompson lead to acetabular erosion, highlighting the need to address both sides of the joint
-In 1950s: Ring, McKee-Farrar created the first Total Hip Arthroplasty, a metal-on-metal devise, which had too high friction causing early loosening.
-In 1950s: The modern version of a Total hip Arthropasty began with the works of Sir John Charnley, who transformed the procedure into a reliable and reproducible treatment for hip arthritis. He is probably best known for pioneering poly liners and cement fixation.
-First to use cold-curing acrylic cement (polymethylmethacrylate, PMMA).
-“Low frictional torque arthroplasty”. Recognized that high forces on the implant was the major contributor to loosening. In searching for low friction material combinations, he found that a stainless steel ball on polytetrafluoroethylene had a coefficient of friction similar to the normal joint. He additionally decreased the femoral head size from 40 mm (which was the Moore type) to 22 mm (reducing the contact area and thus the frictional force). Although decreasing surface area increases the pressure on the implant, he believed the key to longevity lay in reducing friction, and thus torque on the implant.