Venous thromboembolism (VTE) refers to abnormal coagulation that develops into deep venous thrombosis (DVT) and/or pulmonary embolism (PE).
Normal hemostasis is maintained as a balance between Coagulation (clot formation) and Fibrinolysis (clot breakdown) pathways. Coagulation is driven by the Intrinsic Pathway ("contact activation" when damaged to blood vessels expose sub-endothelium to Factor 7) and the Extrinsic Pathway (activated when damaged cells release a burst of Tissue Factor). Coagulation Cascade converges on Fibrin. Fibrin forms a sticky mesh (think spiders web) to trap the circulating platelets and form a clot. The Fibrinolytic system promotes blood flow by activating Plasmin. The competing activity of Fibrin and Plasmin is balanced unless the Coagulation Cascade is promoted via Virchow Triad (stasis, endothelial damage, up-regulation tissue factors).
Arthroplasty procedures upset normal hemostasis, and therefore, VTE prophylaxis is recommended by AAOS [1] and ACCP (American College of Chest Physicians) [2]. THA patients are at higher risk for symptomatic PE compared to TKA, but lower risk for overall DVT.
A multimodal approach using both pharmacotherapy and mechanical prevention is recommended [3]. Overall these recommendations are broad, with many medications available and a wide variety of protocols [4]. The dictum that you see a lot of treatment options when there is no good treatment option appears to be part of the story with DVT prevention. The rate of DVT decreases significantly with prophylaxis, yet the rate of overall DVT remains surprisingly high (20 -40%) when all patients are routinely scanned. The rate of symptomatic DVT is considerably lower (~5%) and the rate of symptomatic PE is still lower (~1%). The wide variation in these numbers underscores the challenge in distinguishing which are significant. The uncertainty about what to do with this information is why routine screening is broadly discouraged. At this time its believed that asymptomatic DVTs should be ignored, while symptoms associated with DVT should prompt a doppler ultrasound, and positive findings should be treated as a symptomatic DVT (see complications section). Symptomatic DVTs pose their own complications (postthrombotic syndrome), and there is a correlation between proximal DVTs and increased risk of propagation.
Further complicating the matter, one study examined the literature for efficacy of pharmacologic agents in DVT prophylaxis and found 73% were industry sponsored with 96% reporting favorable outcomes, while the few studies that were not funded showed significantly less impressive outcomes, with 20% showing the studied medication was either not effective or not safe [5]. Addtionally, it remains debatable whether patients comply fully with the recommendations. Friedman et al. reported in the GLORY study that only 62% THA and 69% TKA patients complied with medications [6].
VTE prophylaxis recommendations by AAOS:
Current recommendations suggest pharmacologic anticoagulation for 14 days in low risk patients following TJA, and up to 35 days in higher risk patients, in combination with mechanical compression.
VTE prophylaxis recommendations by CHEST:
2.1.1 In patients undergoing THA or TKA we recommend use of one of the following for a minimum of 10 to 14 days rather than no antithrombotic prophylaxis: LMWH, fondaparinux, apixaban, dabigatran, rivaroxaban, unfractionated heparin, warfarin, aspirin (all grade 1B), or an intermittent pneumatic compression device (grade 1c).
Mechanical Compression.
Sequential compression devices for calf or foot increase peak venous flow to reduce stasis and up-regulate the fibrinolytic pathway. Independently reduce risk of VTE [7] [8] [9]. Japanese study examined over 2,000 TJA patients and 45% received only mechanical prophylaxis. These patients had the same VTE rate by Doppler as lovenox or heparin groups (roughly 26%) %) [10]. Another Asian study similarly looked at mechanical compression alone. [11], [12]
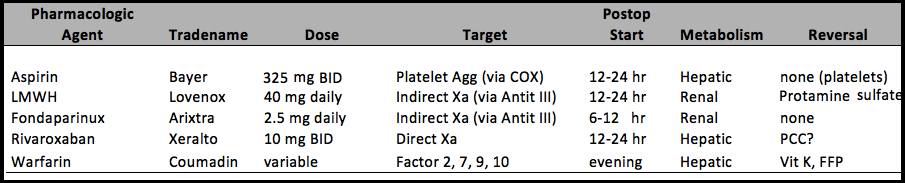
Aspirin
Irreversible direct inhibitor of COX pathway in platelets, preventing Thromboxane A2 release (required to make platelets aggregate).
dosing: 325 mg tab BID (vs. 81 mg tab daily) starting 12-24 hrs postop
Aspirin has grown in popularity: 1) due to efficacy of dvt prophylaxis for primary TJA [13-15], and revision cases[16]. 2) reduced risk of bleeding complications [13]; 3) low cost [17]. It is independently associated with shorter length of stay, leading to decreased costs (if you control for length of stay, aspirin no longer leads to cheaper medical care suggesting the INR monitoring is not a significant expense) [18]. It is recognized by ACCP and AAOS as acceptable agent for DVT prophylaxis.
LMWH (low molecular weight heparin) "enoxaparin/lovenox"
Indirect Factor Xa inhibitor. Other Indirect factor Xa inhibitor include Unfractionated Heparin, and Fondaparinux (synthetic form). Binds Antithrombin III and Thrombin (Factor IIa)
dosing: 30 mg BID starting 12-24 hrs postop. In Europe the dosing is 40 mg daily (starting the night before surgery)
Advantages: no monitoring, appears more effective in preventing overall number of DVT, although no difference in preventing symptomatic DVT as compared to warfarin. Risk of bleeding events are similar to warfarin. Superior to Unfractionated Heparin because higher bioavailability (90% vs. 30%), longer half life, lower risk of bleeding.
Renal metabolism. Not recommended with renal insufficiency, not recommended in combination with epidural catheters.
Fondaparinux "arixtra"
Synthetic Indirect Factor Xa inhibitor
dosing: 2.5 mg/day starting 6-12 hrs postop.
Meta-analysis of 4x randomized clinical trials comparing with lovenox indicated it was superior in preventing DVT [19]. Overall there was no difference in bleeding risk, although 1 of 4 trials found worse bleeding in fondaparinux and its use in North America is limited due to that concern [20].
Rivaroxaban "xarelto"
Direct Factor Xa inhibitor. Other direct factor Xa inhibitors include eliquis (apixaban).
dosing: 10 mg daily starting 12-24 hrs postop. Recommended 12 days TKA, 35 days THA.
Advantages: oral medication, no monitoring required. More effective at preventing total VTE, but equal at preventing symptomatic VTE compared with enoxaparin [21]. One study found prolonged dosing (35 days) was significantly more effective at preventing symptomatic VTE as compared to 10-14 days of enoxaparin [22].There is concern about higher bleeding rates leading to more reoperation [23], and there isnt a good reversal agent.
Warfarin (coumadin)
dosing: variable based on INR target starting night of surgery.
A historical standard anticoagulant for DVT prophylaxis due to proven benefit in VTE prevention and reversibility if hemorrhagic complications occur. Recently fallen out of favor due to the wide variation in metabolism among patients, which leads to high variation in INR values. Too often patients are overtreated (INR > 3) or undertreated (INR < 1.5) while the target INR (2.0, not 2.0 – 3.0 which risks bleeding) appears slow to achieve (often 3 days postop) and difficult to maintain for 2 weeks (the challenge of obtaining serial INR adds to patient frustration). Avoid in conjunction with NSAIDS.
Multiple randomized trials have compared warfarin to LMWH and found no difference in preventing symptomatic DVT, although all studies suggest that LMWH is more effective in preventing asymptomatic clots [24-26].
REFERENCES
1. Mont, M.A. and J.J. Jacobs, AAOS clinical practice guideline: preventing venous thromboembolic disease in patients undergoing elective hip and knee arthroplasty. J Am Acad Orthop Surg, 2011. 19(12): p. 777-8.
2. Falck-Ytter, Y., et al., Prevention of VTE in orthopedic surgery patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest, 2012. 141(2 Suppl): p. e278S-325S.
3. Lieberman, J.R. and M.J. Pensak, Prevention of venous thromboembolic disease after total hip and knee arthroplasty. J Bone Joint Surg Am, 2013. 95(19): p. 1801-11.
4. Anderson, F.A., Jr., et al., Prevention of venous thromboembolism after hip or knee arthroplasty: findings from a 2008 survey of US orthopedic surgeons. J Arthroplasty, 2012. 27(5): p. 659-66 e5.
5. Lee, Y.K., et al., Conflict of interest in the assessment of thromboprophylaxis after total joint arthroplasty: a systematic review. J Bone Joint Surg Am, 2012. 94(1): p. 27-33.
6. Friedman, R.J., et al., Practice patterns in the use of venous thromboembolism prophylaxis after total joint arthroplasty--insights from the Multinational Global Orthopaedic Registry (GLORY). Am J Orthop (Belle Mead NJ), 2010. 39(9 Suppl): p. 14-21.
7. Wilson, N.V., et al., Thrombo-embolic prophylaxis in total knee replacement. Evaluation of the A-V Impulse System. J Bone Joint Surg Br, 1992. 74(1): p. 50-2.
8. Warwick, D., et al., A randomised comparison of a foot pump and low-molecular-weight heparin in the prevention of deep-vein thrombosis after total knee replacement. J Bone Joint Surg Br, 2002. 84(3): p. 344-50.
9. Pitto, R.P., et al., Mechanical prophylaxis of deep-vein thrombosis after total hip replacement a randomised clinical trial. J Bone Joint Surg Br, 2004. 86(5): p. 639-42.
10. Migita, K., et al., Venous thromboembolism after total joint arthroplasty: results from a Japanese multicenter cohort study. Arthritis Res Ther, 2014. 16(4): p. R154.
11. Sugano, N., et al., Clinical efficacy of mechanical thromboprophylaxis without anticoagulant drugs for elective hip surgery in an Asian population. J Arthroplasty, 2009. 24(8): p. 1254-7.
12. Park, Y.G., et al., Incidence and Fate of "Symptomatic" Venous Thromboembolism After Knee Arthroplasty Without Pharmacologic Prophylaxis in an Asian Population. J Arthroplasty, 2016. 31(5): p. 1072-7.
13. Raphael, I.J., et al., Aspirin: an alternative for pulmonary embolism prophylaxis after arthroplasty? Clin Orthop Relat Res, 2014. 472(2): p. 482-8.
14. Bozic, K.J., et al., Does aspirin have a role in venous thromboembolism prophylaxis in total knee arthroplasty patients? J Arthroplasty, 2010. 25(7): p. 1053-60.
15. Vulcano, E., et al., Aspirin for elective hip and knee arthroplasty: a multimodal thromboprophylaxis protocol. Int Orthop, 2012. 36(10): p. 1995-2002.
16. Deirmengian, G.K., et al., Aspirin Can Be Used as Prophylaxis for Prevention of Venous Thromboembolism After Revision Hip and Knee Arthroplasty. J Arthroplasty, 2016.
17. Gutowski, C.J., et al., Direct Costs of Aspirin versus Warfarin for Venous Thromboembolism Prophylaxis after Total Knee or Hip Arthroplasty. J Arthroplasty, 2015. 30(9 Suppl): p. 36-8.
18. Lotke, P.A. and J.H. Lonner, The benefit of aspirin chemoprophylaxis for thromboembolism after total knee arthroplasty. Clin Orthop Relat Res, 2006. 452: p. 175-80.
19. Turpie, A.G., et al., Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med, 2002. 162(16): p. 1833-40.
20. Bauer, K.A., et al., Fondaparinux compared with enoxaparin for the prevention of venous thromboembolism after elective major knee surgery. N Engl J Med, 2001. 345(18): p. 1305-10.
21. Eriksson, B.I., et al., Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med, 2008. 358(26): p. 2765-75.
22. Kakkar, A.K., et al., Extended duration rivaroxaban versus short-term enoxaparin for the prevention of venous thromboembolism after total hip arthroplasty: a double-blind, randomised controlled trial. Lancet, 2008. 372(9632): p. 31-9.
23. Wood, R.C., 3rd, et al., Retrospective Evaluation of Postoperative Bleeding Events in Patients Receiving Rivaroxaban After Undergoing Total Hip and Total Knee Arthroplasty: Comparison with Clinical Trial Data. Pharmacotherapy, 2015. 35(7): p. 663-9.
24. Hull, R., et al., A comparison of subcutaneous low-molecular-weight heparin with warfarin sodium for prophylaxis against deep-vein thrombosis after hip or knee implantation. N Engl J Med, 1993. 329(19): p. 1370-6.
25. Francis, C.W., et al., Prevention of deep-vein thrombosis after total hip arthroplasty. Comparison of warfarin and dalteparin. J Bone Joint Surg Am, 1997. 79(9): p. 1365-72.
26. Colwell, C.W., Jr., et al., Comparison of enoxaparin and warfarin for the prevention of venous thromboembolic disease after total hip arthroplasty. Evaluation during hospitalization and three months after discharge. J Bone Joint Surg Am, 1999. 81(7): p. 932-40.