Trunnionosis generates metal debris and causes ARMD (adverse reaction to metal debris). Surgeons performing THA with Metal-on-Poly implants continued to see the classic ARMD (associated with Metal-on-Metal implants) and they found the source of metallosis to be the head-neck Morse Taper ("trunnion"). This is MoM connection within a Metal-on-Poly implant that produce metal debris.
Metals implanted into the body (which is an oxygen-rich environment) avoid corrosion by forming a thin protective layer of metal oxide via the process of passivation (making the metal inert). If this layer is damaged, then re-passivation can occur to re-form the protective layer. Yet two processes can occur at the trunnion to prevent the re-formation of this protective layer - fretting and crevice corrosion.
Fretting.
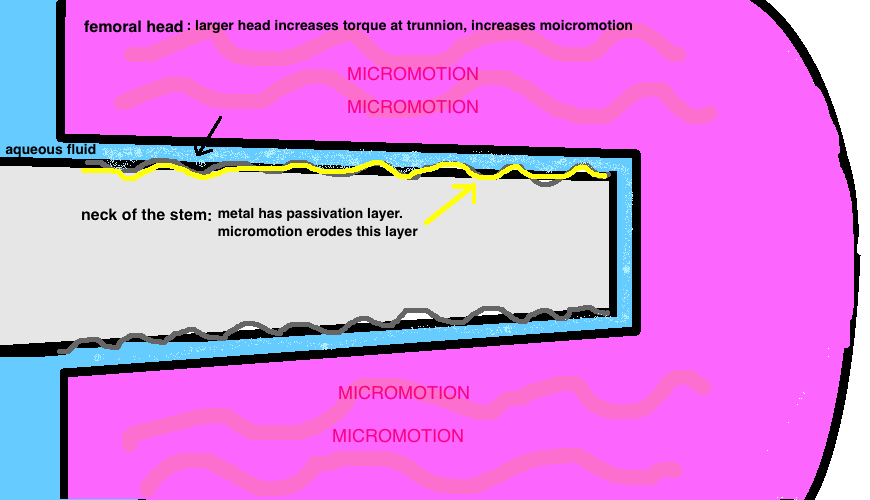
Fretting Corrosion is caused by micromotion
Mechanical micromotion between the neck and head destroys the passive layer. Mild to moderate fretting is seen in about 80% of heads (female side); and 50% of trunnions (male side), meaning this type of wear is fairly common overall.
Fretting appears to be a particular problem in large femoral heads (36 + mm heads) because larger heads create a greater lever arm and increased torque at the trunnion [1]. The excellent wear characteristics of highly-crosslinked poly has allowed the use of larger diameter heads to improve stability without the risks of volumetric wear, however, trunnionosis may be a previously unrecognized side effect.
There is also a direct correlation between increased taper rigidity and decreased fretting. Longer tapers have more contact and more rigidity and less fretting [2, 3]. More head offset (ie a +8) increases the amount of fretting.
Crevice corrosion.
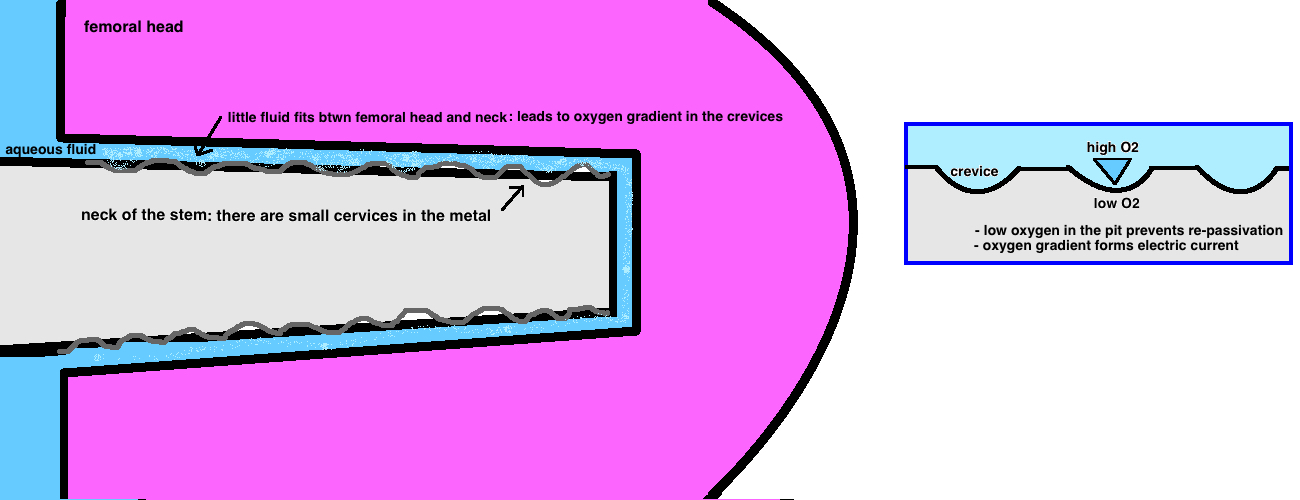
Crevice Corrosion prevents reformation of the passive layer
The normal aqueous fluid circulating in our tissue cannot fully penetrate the tight space formed by the trunnion, and this causes small crevices (between the head and neck along the trunnion) to be isolated from the surrounding chemical environment. The bottom of these crevices are "hypoxic" while the top of the crevice is exposed to normal fluid and are "normoxygic" and this gradient in effect creates an electric current (theres an anode and cathode) even though the metals are the same (in cases of dissimilar metals, this problem is much worse). These oxygen-poor "pits" also cannot re-form the protective layer (which requires oxygen to repassivate) and crevice corrosion thus occurs.
Black substance.
Phosphate in the aqueous fluid reacts with the chromium to form a black precipitate. Because the chromium precepitates out, the serum levels are often normal, while the cobalt is more soluble and will elevate in the blood. In contrast, a MoM articulation will often produce elevated serum levels of both chromium and cobalt.
Standardization.
Retrieval studies examined the head-neck junction of multiple THA designs and have identified varying degrees of corrosion. Currently there is no standardization of the Morse Taper in THA despite being around THA for over three decades. Studies have shown variations in the surface roughness (distance of peaks and troughs) which correlate directly to risk of corrosion [4].
Dual Modular Design.
The risk of metal wear is particularly elevated in the “dual modular designs” (meaning that there is a junction at both the head-neck and the neck-body). These dual-articulation designs expose the implant to more motion that can generate wear particles. There was a dramatically increased incidence of ARMD in some implants [5], and some (ie Stryker ABG II /Rejuvinate) were voluntarily recalled.
REFERENCES
1. Livermore J et al. Effect of femoral head size on wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990 Apr;72(4):518-28.
2. Goldberg JR et al. A multicenter retrieval study of the taper interfaces of modular hip prostheses. Clin Orthop Relat Res. 2002 Aug;(401):149-61.
3. Porter DA et al. Modern trunnions are more flexible: a mechanical analysis of THA taper designs. Clin Orthop Relat Res. 2014 Dec;472(12):3963-70.
4. Munir S. Variations in the trunnion surface topography between different commercially available hip replacement stems. J Orthop Res. 2015 Jan;33(1):98-105. doi: 10.1002/jor.22741. Epub 2014 Oct 15.
5. Cooper, H.J., The local effects of metal corrosion in total hip arthroplasty. Orthop Clin North Am, 2014. 45(1): p. 9-18.