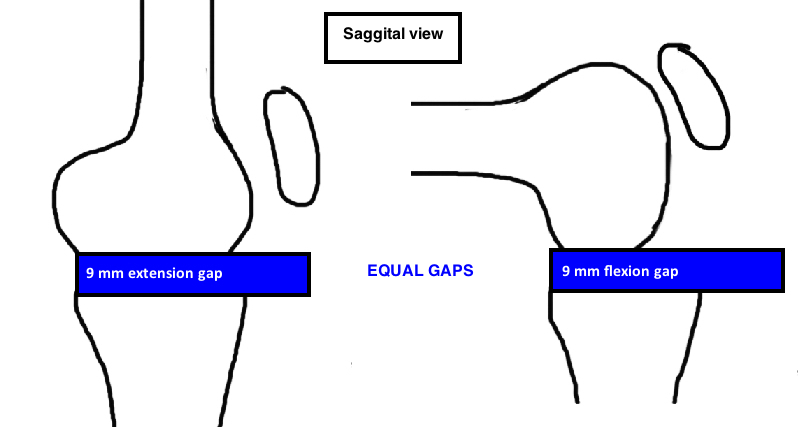
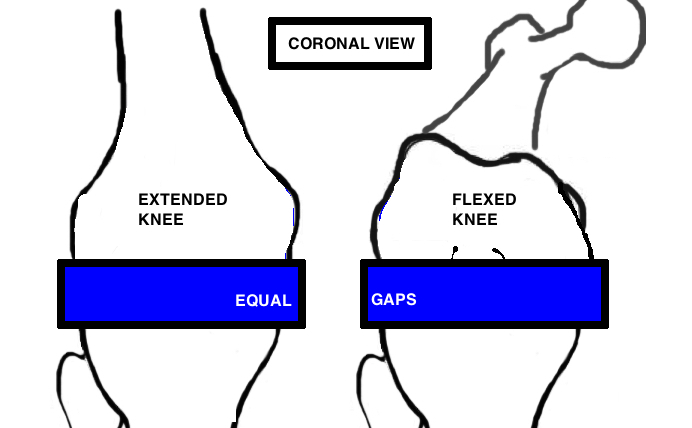
One goal of TKA is to achieve balanced tension within the knee throughout range of motion. This balanced tension is important for implant stability and longevity .
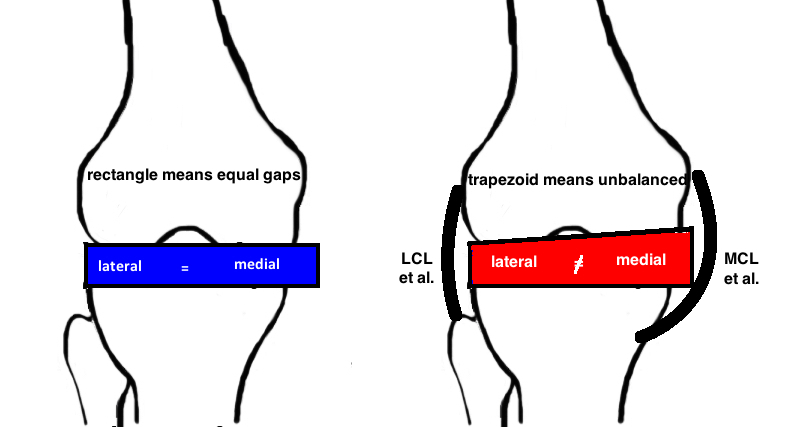
A balanced knee has rectangular Flexion and Extension gaps - the rectangle demonstrates that the medial and lateral compartment share equal tension. A trapezoid means that one side is looser (aka "opening up") and therefore, this side will experience less tension and this may cause an unstable TKA and/or asymmetric wear and early failure.
The angle of bone cuts and the surrounding soft tissue tension can both affect the balance of the flexion gap (90°) and extension gap (0°).
The balance of a gap is measured with a spacer block.
A balanced knee has equal sized Flexion and Extension gaps. A balanced knee has rectangular Flexion and Extension gaps.
In the perfect world, you cut the femur, you cut the tibia and the result is a perfect rectangle for the Flexion and Extension Gap. But in reality, trapezoidal flexion and extension gaps occur despite perfect bone cuts because of soft tissue imbalance.
As a knee develops arthritis, it typically develops a concomitant deformity of either varus or valgus. Over time, this deformity affects the tension of the ligaments around the knee. A Varus Deformity (90% of cases) causes the lateral ligaments to stretch, while the medial ligaments are taken off tension and become tight and stiff. A Valgus deformity places stress on the medial ligaments and causes them to become stretched, while the lateral ligaments are off tension and become tight.
The standard approach of Soft Tissue Balancing is to achieve equal medial and lateral tension at 0° and 90°. These two reference points (0° & 90°) are used because its technically easiest for surgeons during the procedure, but the goal is to stabilize the knee throughout the full range of motion (every degree from 0° - 130°). Its clearly impractical to attempt to balance the knee every 5°, yet the question remains whether these 2 check points are sufficient to ensure a balanced knee.
The soft tissue is balanced in the knee by performing "releases" which take tension off the tight structures and allow that side of the gap to open up to match the other side (there are also reports of "tightening" the loose soft tissue, however, the results are less reproducible).
Varus correction.
Medial side is tight. Structures to release include anterior structures that affect flexion gap, and posterior structures that affect extension gap. And this makes sense when you think of flexion as the knee opening up in the front (hinged from the back) and therefore, structures in the front (anterior) will become tight. The opposite, whereby extension hinges from the front and opens in the back, will show posterior structures tight in extnesion. Anterior is superficial MCL. Posteriorly you will release the posterior oblique ligament, and the Semimembranosis, and remove any osteophytes as well.
Valgus Correction.
Only 10% of knee deformities that require TKA are done for the valgus knee. The Ranawat classification [1] uses 3 grades to describe valgus deformity severity. Grade I is <10° valgus deformity (normal valgus angle is ~ 6°), correctable alignment with stress, and intact MCL and this type accounts for >80% of all valgus knees. Grade II is an angle 10° - 20° degrees, MCL is attenuated but a firm endpoint, and this type accounts for 15% of valgus knees. Grade III is a valgus angle >20° and absent or severely attenuated MCL. This grading scale helps to determine the type of implants and correction that is required.
Soft tissue considerations.
If the MCL is intact, then a primary TKA poly insert can be used. If the MCL is elongated, a constrained poly may be necessary to give sufficient coronal stability. Literature shows there is a risk of recurrent valgus deformity after primary TKA when the MCL is deficient and primary insert is used (even when satisfactory ligament balancing occurs at the time of surgery) [2]. The use of constrained poly effective prevents this recurrence [3]. A constrained insert absorbs more of the joint reactive forces, and the next question is whether stems are necessary to increase the surface area of the bone-implant interface to absorb these greater forces [4]. Some argue that an elongated MCL is still functional and a constrained insert without stems is not at increased risk for loosening. If the MCL is completely absent, a hinge prosthesis should be considered as excessive stress to a constrained insert may cause significant wear and early loosening and post fracture.
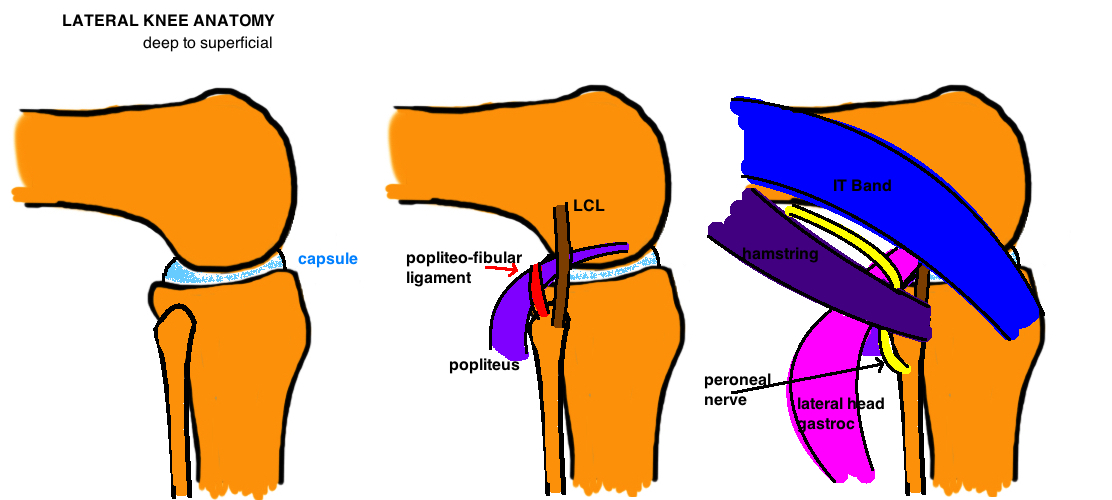
MCL attenuation also adds significant challenge to gap balancing. In a varus knee, the tight medial structures are released to match the normal or slight attenuated lateral side (the point is that the lateral side is rarely significantly loose). In the valgus knee however, the MCL can be significantly pathologic, and by releasing the lateral structures to match the enlongated MCL, you can significant increase the size of the gap (because you are using a very pathologic structure as your target), and you may even lengthen the operative leg, require a large poly, and put the peroneal nerve at risk for traction injury.
There is debate about the order of soft tissue releases to achieve a balanced gap. Releases should be performed with the knee in extension and the balance should be rechecked after every release. Ranawat recommends “inside-out” technique of pie-crusting the IT band, then the LCL with a no. 15 blade, and making effort to preserve the popliteus. [1] The peroneal nerve is at risk between IT band and Popliteus at the level of the tibial cut. Studies show that LCL release provides the most correction, and some recommend releasing first in cases of severe valgus deformity [5] [2].
Bone considerations.
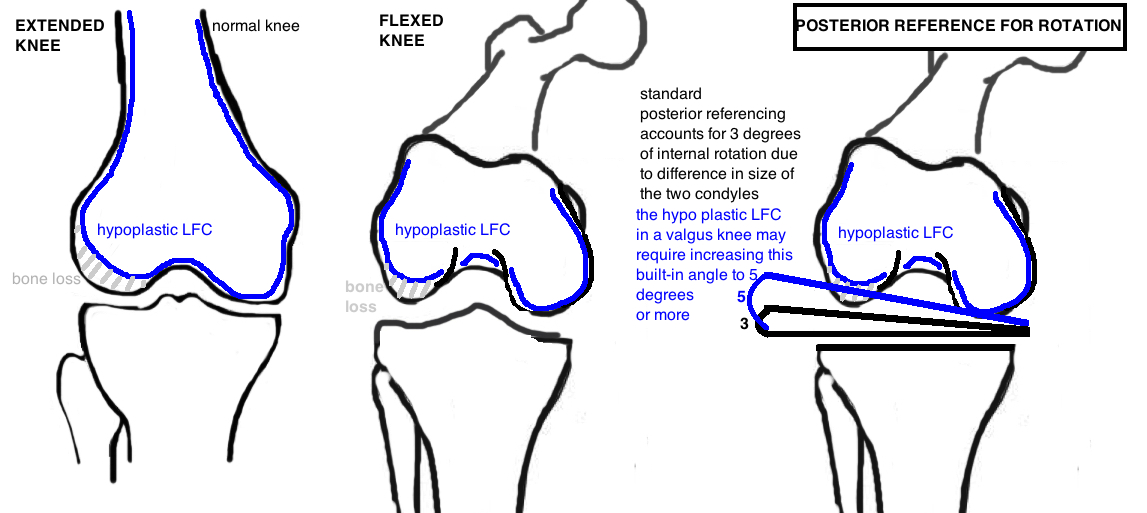
The valgus knee is uniquely different from the varus knee because bone loss occurs on the lateral femur (in contrast to vaurs knee that shows anterior-medial tibial bone loss. The entire Lateral Femoral Condyle can be significantly hypoplastic (posterior and distal femoral condyles). This is important to identify if the surgeon is measuring femoral rotation by posterior referencing, which typically add 3° to compensate for the difference in sizes between the medial and lateral femoral condyle. In the case of a hypoplastic LFC, the posterior referencing system may need to dial in 5° or more to prevent internal rotation of the femoral component. Additionally, if there is more than 5 mm of deficient bone on the posterior or distal femoral cut, augments should be considered because a cement mantle this large will lead to early loosening. It is important not to chase a large bone defect. If the distal femoral cut does not touch the lateral femur, do not resect additional distal femur because this will raise the joint line, causing patella baja. Similarly, if there is tibial bone loss, measure 4-6 mm off the medial side (non-affected side) to determine the depth of the cut, attempting to cut distal to the defect often removes excessive bone (“apb”: always preserve bone!). The distal femoral cut is often made at only 3° as opposed to the standard 5 – 7° to avoid under-correction of the deformity.
Balancing the Flexion and Extension Gap
Academic versus Practical Gap Balancing.
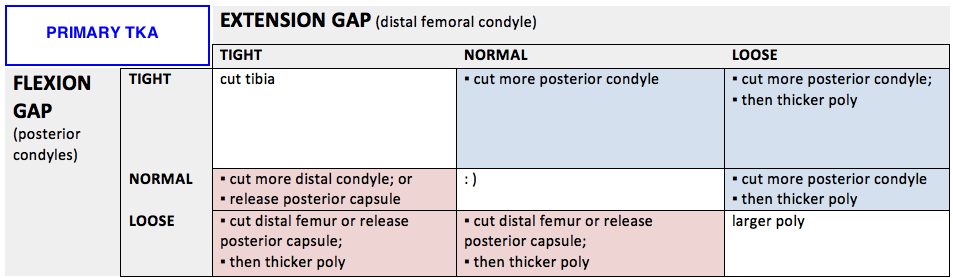
We have all studied this gap balancing matrix. And conceptually it is helpful. But many of the squares in this chart recommend "augments" to treat flex-ext imbalance which is almost never done for a primary TKA in reality (revision TKA is a different story). Therefore the gap balancing techniques should be understood as slightly different in the primary and revision setting.
In the primary setting, it is uncommon to see dramatic differences in flexion and extension if the bone cuts were done properly so lets throw augments out the window and see whats left. When differences between flexion and extension are small, we can make some generalizations and therefore simplify the options. A tight flexion gap and a loose extension gap is similar. If we are not considering augments, we can only focus on increasing the flexion gap (theres nothing we can do about reducing the extension gap). So what are the options for a tight flexion gap: 1) cut more posterior femoral condyle. much simpler right. Lets look at the converse: a tight extension gap and a loose flexion gap is similar. Again, we are not considering augments for the loose flexion gap, so we can think of this problem also as a tight extension, which has 2 options: 1) cut more distal femoral condyle; 2) release posterior capsule. Generally its preferred to first release posterior capsule because this doesnt affect the joint line.
In the revision setting, there is greater variability in the gap mismatch, there is often significant bone loss and therefore, distal femur or posterior condyle augments are frequently a good option. Thus, the more academic gap balance matrix can be used with all its varying options.
REFERENCES
1. Ranawat, A.S., et al., Total knee arthroplasty for severe valgus deformity. J Bone Joint Surg Am, 2005. 87 Suppl 1(Pt 2): p. 271-84.
2. Favorito, P.J., W.M. Mihalko, and K.A. Krackow, Total knee arthroplasty in the valgus knee. J Am Acad Orthop Surg, 2002. 10(1): p. 16-24.
3. Easley, M.E., et al., Primary constrained condylar knee arthroplasty for the arthritic valgus knee. Clin Orthop Relat Res, 2000(380): p. 58-64.
4. Anderson, J.A., et al., Primary constrained condylar knee arthroplasty without stem extensions for the valgus knee. Clin Orthop Relat Res, 2006. 442: p. 199-203.
5. Krackow, K.A. and W.M. Mihalko, Flexion-extension joint gap changes after lateral structure release for valgus deformity correction in total knee arthroplasty: a cadaveric study. J Arthroplasty, 1999. 14(8): p. 994-1004.