Patellar Tendon Rupture
Patellar tendon rupture is a serious complication with generally poor results. Direct repair of the tendon has very poor outcomes (<50% success with suture or staple)[65, 66], and therefore a rupture requires reconstruction (like a torn ACL). Reconstruction options include autograft, allograft, or synthetic mesh. Overall the functional outcome results are inconsistent and highly variable.
Autograft. Similar to an ACL autograft reconstruction, the semitendinosis can be harvested and used as the patellar tendon reconstruction [67].
Technique. Instead of removing the tendon at its insertion on the pes, the tendon is mobilized but not detached, and a tendon stripper is then used to release the tendons from their muscular attachment proximally. The tendons are then wrapped through the patella (typically if just the SemiT is used, it can fit into a 6 mm tunnel in the distal 1/3 of the patella) and it is then re-attached onto the proximal tibia with the knee at 90° flexion to ensure proper patellar height. The knee is then immobilized in extension for 6 weeks, followed by limiting knee flexion to 60° for 12 weeks, followed by progressive knee motion. This is the standard surgical treatment for a chornic patellar tendon rupture in the native knee, which good long term outcomes. The technique however is less effective in the TKA due to the patellar bone loss from its resurfacing.
Allograft. The allograft technique uses either an Achilles (with calcaneal bone block) or Whole Extensor Mechanism (quad tendon-patella-patellar tendon-proximal tibia) graft. The graft is an afibrous network that allows for fibrous ingrowth.
Technique. The Whole Extensor Mechanism graft requires 5 cm of proximal bone stock and 5 cm of quad tendon. When implanted, the graft must be placed under maximal tension with the knee in extension (and don’t test the graft afterward). Tensioning majorly decreases the residual extensor lag, which is the primary mode of failure for these grafts. The graft is either placed over the anterior surface of the extensor mechanism (“onlay technique”) or threaded into the extensor mechanism through the lateral retinaculum (like a pulver-taft weave). The knee is then immobilized in a cast for 6 weeks. The allograft has good integration into host tissue, yet there are many failures (about 35% early failure and close to 50% at 10 years) [68, 69]. Most are functional failures as defined as an extensor lag > 30°.
Mesh. Browne and Hanssen reported a technique using Marlex Mesh (a high density polyethyene fiber typically used for hernia repairs in abdnomial surgery) to recreate the extensor mechanism after a patellar tendon rupture [70]. The concept is that mesh promotes extensive scar tissue formation that provides strength and resists creep, which commonly leads to failure in the allograft technique. The initial paper reports good outcomes in 9/13 patients, with 3 early re-ruptures and 1 infection.
Technique. Fold the mesh several times until it’s a width of 2 – 2.5 cm, and then secure to the tibia by creating a trough proximal and slightly lateral to the tibial tubercle and fixed the mesh with a screw, and then cemented it in place. If the tibial component is being revised at the time, the mesh can be placed into the tibial canal and then implant cemented over it. The mesh then runs under the remaining patellar tendon, through the lateral retinaculum, is then fixed to the patella, and then sutured to the quad tendon and vastus lateralis with non-absorbable sutures with the knee in extension. Then VMO is then mobilized and sutured on top of the mesh to create a "mesh sandwich". The knee is kept in extension for 6-8 weeks and then 10° of knee flexion is advanced each week.
Patella Fracture
Patellar fracture is an uncommon problem, occurring less than 0.5% of cases.
Fracture is closely associated with patellar bone stock. Increased risk of fracture is associated with < 12 mm of native patella after resurfacing. The incidence of fracture in non-resurfaced patella is only 0.05%. Patella fracture is also associated with AVN. Disruption of the anastomotic ring around the patella can lead to AVN and then fracture. Increased risk for AVN is associated with lateral release for patellar tracking and the V-Y turndown for exposure in revision cases. The prosthetic designs more commonly associated with fracture are the single peg versus the tri-peg fixation. Also, femoral components with a thicker anterior flange. Malrotated femoral component can also place excessive force across the patella.
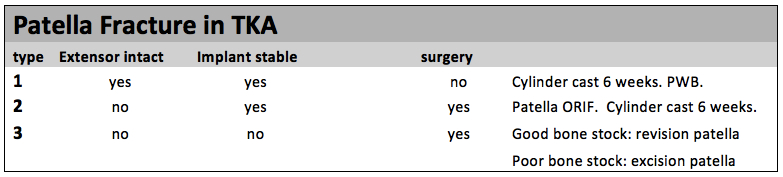
Treatment is determined by whether the extensor mechanism is intact, and whether the implant is stable. [58].
Type 1: Stable implant and extensor mechanism is intact. Treat nonoperatively with protective weight bearing and a cylinder cast for 6 weeks.
Type 2: Disrupted extensor mechanism but stable implant, which requires surgical treatment to ensure return of extensor function. These are challenging because the tension band is less effective as when used in native patella fractures. The patellar component prevents the conversion of the tension force to a compressive force so you cannot get the same level of healing. Need to cast for 6 weeks after fracture regardless of fixation technique.
Type 3: Loose components, surgery is recommended but treatment decision further depends on bone stock. With good bone the implant can be revised (possibly using a tantalum patella), while in poor bone (< 10 mm thickness or comminution) may require patellar excision.
Patella Instability
Patellar mal-tracking is caused by tibia or femoral mal-rotation (internal rotation). Its symptoms are often vague: anterior pain, instability, stiffness, weakness, locking and giving out. It is most commonly observed in valgus knees (large Q angles), obese patients, malrotated componenets, asymmetric patellar resection. If surgery is required, the internally rotated components should be revised to maximize improvement. Lateral release is often used to decrease lateral directed tension to decrease dislocation risk.
Patellar Clunk
The Patellar Clunk Syndrome is a painful clunk sensation when the knee is brought into extension and is associated with scar tissue in the suprapatellar pouch that becomes trapped in the femoral notch at 30° flexion. The problem has mainly been resolved with newer designs that alter the trochlear groove, however, patients with older design TKA can be treated effectively the arthroscopic debridement.
References
1. Ortiguera, C.J. and D.J. Berry, Patellar fracture after total knee arthroplasty. J Bone Joint Surg Am, 2002. 84-A(4): p. 532-40.
2. Rand, J.A., B.F. Morrey, and R.S. Bryan, Patellar tendon rupture after total knee arthroplasty. Clin Orthop Relat Res, 1989(244): p. 233-8.
3. Lynch, A.F., C.H. Rorabeck, and R.B. Bourne, Extensor mechanism complications following total knee arthroplasty. J Arthroplasty, 1987. 2(2): p. 135-40.
4. Cadambi, A. and G.A. Engh, Use of a semitendinosus tendon autogenous graft for rupture of the patellar ligament after total knee arthroplasty. A report of seven cases. J Bone Joint Surg Am, 1992. 74(7): p. 974-9.
5. Burnett, R.S., et al., Retrieval of a well-functioning extensor mechanism allograft from a total knee arthroplasty. Clinical and histological findings. J Bone Joint Surg Br, 2004. 86(7): p. 986-90.
6. Burnett, R.S., et al., Extensor mechanism allograft reconstruction after total knee arthroplasty. A comparison of two techniques. J Bone Joint Surg Am, 2004. 86-A(12): p. 2694-9.
7. Browne, J.A. and A.D. Hanssen, Reconstruction of patellar tendon disruption after total knee arthroplasty: results of a new technique utilizing synthetic mesh. J Bone Joint Surg Am, 2011. 93(12): p. 1137-43.