Clinically relevant stiffness occurs in about 5% of TKA cases. It can be caused by pain, component malpositioning/malsizing, or arthrofibrosis. Flexion contracture (ie loss of terminal extension) is the least tolerated limitation in motion because >5-8 ° affects the gait pattern and prevents patients from locking out their knee while standing, leading to increased muscle fatigue bc the quad never gets a chance to relax. Terminal flexion is important for daily activity: 67° flexion is needed for the swing phase of walking, 100° to descend stairs, 105° to rise from chair.
A TKA rarely achieves the terminal flexion of a native knee…so when do we say the TKA is clinically stiff? The definition of stiffness has been a moving target over the past few decades with limitations to knee motion becoming less and less acceptable. Generally speaking, flexion less than 90° is considered stiff. Stiffness is often very painful and causes significant functional disability. It is closely related to patient satisfaction after TKA. Risk factors include: young age, limited pre-op ROM, female, poor post-op pain control.
Treatment.
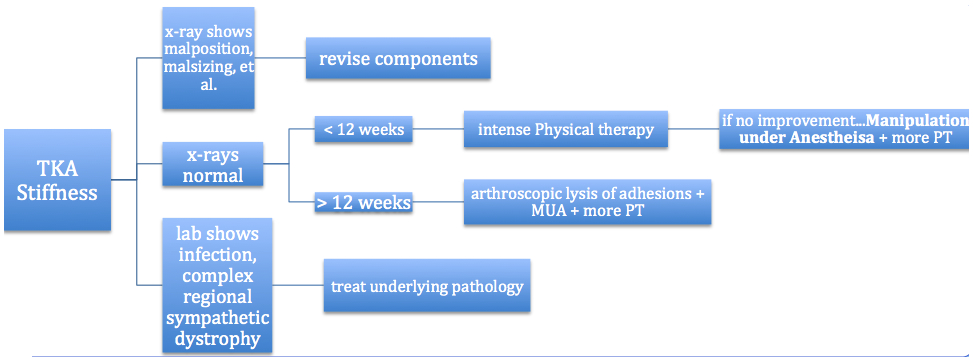
The key is to first identify the underlying cause. Soft tissue contractures should be a diagnosis of exclusion. Before associating the limited motion with soft tissue, its important to rule out infection, complex regional pain syndrome, and gross malpositioning or malsizing of the components. Malrotation causes an asymmetric flexion gap, and can lead to lift-off and issues with patellar tracking that decreases flexion. Furthermore, a tight flexion gap due to oversized femoral component or a tight PCL with a CR-TKA, or a tight patellofemoral joint that causes the retinaculum to tighten with flexion leading to anterior knee pain, or patella baja (the patella articulates with the PE liner causing a block to motion) can all prevent terminal flexion and require separate intervention. If these causes are ruled out, and soft tissue appears to be the cause of limited motion, then a number of treatments are recommended in a sequential manner (see figure). To assist in understanding the best treatment, consider the severity of limited motion, if there are technical errors from surgery (best evaluated with a CT scan), if there are patient factors that cannot be modified (ie morbid obesity, major limitation to motion preop, RSD, etc).
Physical Therapy. Many patients fail to progress due to poor physical therapy, or poor postoperative pain control. Improving pain control and putting patients onto a strict PT regimen can often lead to meaningful gains, when the issue is identified early. The sooner the better, and aggressive PT is best within 6 weeks for flexion or extension bracing for incomplete extension. Gains from therapy are best in cases of good pre-op motion, small contractures, and relatively good pain control.
Continuous Passive Motion: Gains from a CPM machine are not well supported in the literature.
Manipulation under anesthesia (MUA). MUA is considered for those that fail to achieve 90° by 6-12 weeks postop. Beyond 12 weeks, MUA has not proven an effective treatment and it increases the risk for fracture or extensor mechanism injury. The main indication is for limited flexion, yet limited extension is a more common and more refractory soft tissue contracture (MUA for > 10° lost extension is associated with notable risk for supracondylar fracture and should be avoided). The goal of MUA is > 115° flexion with gravity alone. The technique involves gradually increasing pressure to the knee over 5 to 15 minutes. Intra-op, gravity alone ROM should be documented with a goniometer and lateral photograph. After the procedure and before discharge, check that straight leg raise is intact. Consider a femoral or epidural catheter for postop pain relief because all patients should begin rigorous physical therapy immediately postop. Outcomes are encouraging. At an average of 9 weeks post-intervention, the average knee gained 35° flexion and 90% maintained this improvement and continued to improve over the first few months. One study that compared MUA to patients that refused and elected for therapy alone showed a difference in improvement of 33° to 3° (MUA is 10x better). Remember that the best outcomes are for painless, stiff TKA, and that significant pain is often an indication of another underlying diagnosis that needs to be addressed before treating the stiffness. Diabetes or obesity are negative predictors for improvement with manipulation. Furthermore, patients with significant preoperative stiffness show regression after a manipulation, with motion approaching preoperative values at one year.
Arthroscopic Lysis of Adhesions (LOA). This surgical option is typically reserved for recurrent stiffness after failed MUA, or stiffness beyond 3 months (by this time, scar becomes very strong and manipulation increases the risk for fracture or extensor mechanism injury). Results are best for a painless and stiff TKA. Resection of excessive scar tissue in the suprapatellar pouch, and medial/lateral gutters can lead to significant gains. Outcome studies report improvement of up to 36° flexion, and 7° extension (which is often better than MUA).
References
1. Namba, R.S. and M. Inacio, Early and late manipulation improve flexion after total knee arthroplasty. J Arthroplasty, 2007. 22(6 Suppl 2): p. 58-61.
2. Fitzsimmons, S.E., E.A. Vazquez, and M.J. Bronson, How to treat the stiff total knee arthroplasty?: a systematic review. Clin Orthop Relat Res, 2010. 468(4): p. 1096-106.
3. Berger, R.A., et al., Malrotation causing patellofemoral complications after total knee arthroplasty. Clin Orthop Relat Res, 1998(356): p. 144-53.
4. Kim, J., C.L. Nelson, and P.A. Lotke, Stiffness after total knee arthroplasty. Prevalence of the complication and outcomes of revision. J Bone Joint Surg Am, 2004. 86-A(7): p. 1479-84.
5. Gandhi, R., et al., Predictive risk factors for stiff knees in total knee arthroplasty. J Arthroplasty, 2006. 21(1): p. 46-52.
6. Bedard, M., et al., Internal rotation of the tibial component is frequent in stiff total knee arthroplasty. Clin Orthop Relat Res, 2011. 469(8): p. 2346-55.
7. Keating, E.M., et al., Manipulation after total knee arthroplasty. J Bone Joint Surg Am, 2007. 89(2): p. 282-6.
8. Esler, C.N., et al., Manipulation of total knee replacements. Is the flexion gained retained? J Bone Joint Surg Br, 1999. 81(1): p. 27-9.
9. Cates, H.E. and J.M. Schmidt, Closed manipulation after total knee arthroplasty: outcome and affecting variables. Orthopedics, 2009. 32(6): p. 398.
10. Baker, P.N., et al., The role of pain and function in determining patient satisfaction after total knee replacement. Data from the National Joint Registry for England and Wales. J Bone Joint Surg Br, 2007. 89(7): p. 893-900.