Incision
The vascular supply to the skin around the knee is rather tenious due to the lack of underlying muscle or intramuscular septum to allow for arterial perforators, and thus the skin relies on an anastamotic ring within the subcutaneous fascia. The majority of these subq arterioles originate medially: the saphenous artery and the lateral geniculate artery provide medial blood supply.
If there are multiple skin incisions, using the lateral incision will minimize the risk of vascular compromise and wound dehiscence (because the lateral aspect of the wound will have decreased oxygenation and thus its key to not disrupt any further perfusion).
If you need to make a new incision, near an prior incision, a skin bridge of 6 cm is ideal. Avoid a skin incision that intersects prior incisions at acute angles the skin at this junction will be hypoxic.
If the skin quality is poor, if there are many prior incisions, it may be wise to consult a plastic surgeon for muscle flap coverage, or tissue expanders.
Full thickness skin flaps must be made to avoid devasularizing the skin (which is often quite thin). The arthrotomy should be offset from the skin incision to prevent direct pathway to the external environment.
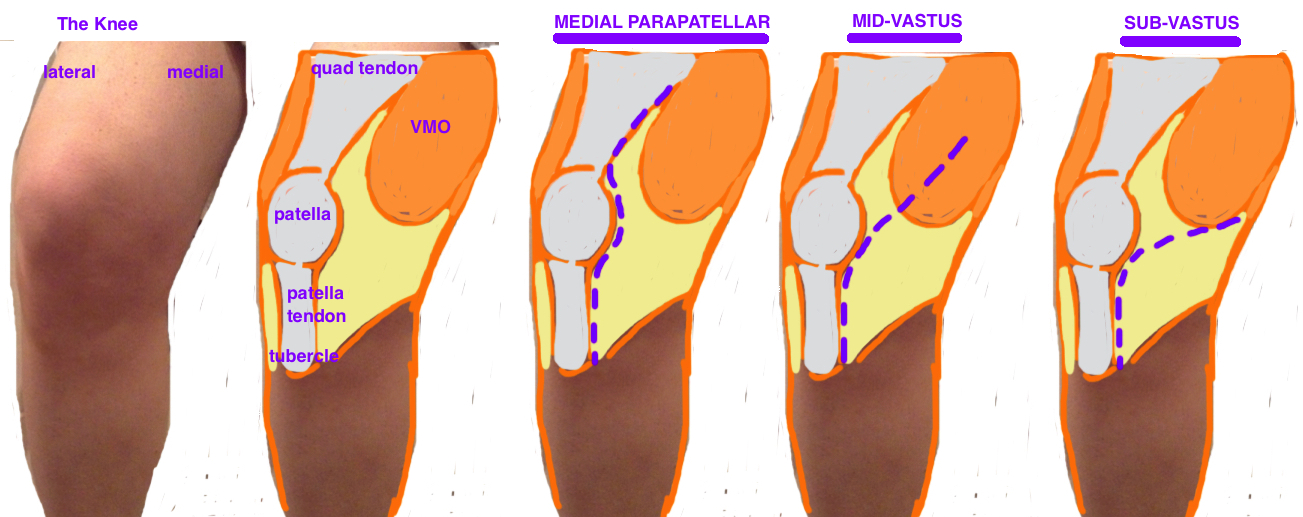
Medial Parapatellar. The goal standard for TKA arthrotomy, initially credited to von Langenbeck. Start midline over knee 2 finger-bredths above patella to 1 cm below tibial tubercle. The VMO is detached from its insertion into the quad tendon, leaving a cuff of tendon (~5 mm) attached to the VMO proximally and a cuff of tendon attached to the medial edge of the patella distally to facilitate repair at closure. The patella is either dislocated or dislocated + everted. There is no definitive evidence to suggest that one technique leads to delayed recovery.
The term for "minimally invasive" doesn't just relate to the size of the incision (although this plays a role) but most importantly, it refers to the amount of soft tissue injury. The goal of the midvastus, subvastus discussed below is to avoid violating the quad tendon [2]. A minimally invasive median parapatellar approach has also been developed which avoids violation of the quad tendon by stopping the proximal extent of the incision at the superior pole of the patella [3]. This limited arthrotomy creates a “mobile window” whereby the entire joint is not visible at once, but rather the incision must be moved during the steps of surgery to expose the necessary bone.
Subvastus (and “mini-subvastus”).
This approach is promoted as an “extensor-mechanism preserving” arthrotomy by staying below the VMO, avoiding an incision into the quad tendon [4].
Some studies suggest that it improves postop quad recovery and reduces pain, while other studies argue that it not only offers no short-term/long-term benefit, but also increases complications due to the reduced visualization of the knee (this approach is not recommended in knees with significant deformity or in obese patients.
Midvastus (and “mini-midvastus”). This approach is a type of compromise between the parapatellar and subvastus, as it violates less of the quad tendon, yet provides improved visualization to the subvastus. The proximal arthrotomy splits thru the VMO muscle fibers. The standard midvastus muscle split goes to the intermuscular septum while the mini approach only violates 2-3 cm of VMO [5].
Extended Approaches (Revision).
Quad Snip. This technique extends the standard medial parapatellar approach by creating a 45° oblique incision proximally across the quad tendon toward the vastus lateralis. This technique is sometimes necessary in revision knees that are stiff. At 30 months, there is no appreciable quad strength deficit compared to a standard medial parapatellar approach [6].
V-Y Turndown (Coonse & Adams). This technique extends the Quad Snip by creating an inverted-V via an oblique incision aimed distal and lateral from the apex of the Quad Snip, which parallels the vastus lateralis. This completely mobilizes the patella, however, it also significantly increase the risk of patellar AVN, and is associated with a 10 - 20° extensor lag.
Tibial Tubercle Osteotomy. Expose in a stiff knee can place significant tension on the patellar tendon insertion, and risk the dreaded complication of a patellar tendon avulsion. A controlled mobilization of the patellar tendon offers great visualization and prevents the risk of iatrogenic tendon rupture in the revision setting. The tubercle osteotomy is typically 5 cm in length, tapers distally, and hinges on the lateral anterior cortex. It is fixed into position with cerclage wires.