The cementless stem obtains initial stability via “press-fit” allowing "bone ingrowth" of the porous-coating by six weeks post-op.
1. rigidity is the short-term goal.
Eventually the implant is stabilized by bone growing into its porous surface, but this takes a few weeks to occur, so how are patients allowed to immediately walk on their implant after surgery? Initial implant rigidity is achieved via “Press-Fit”, which is rigid contact between the implant and the weight bearing cortical bone (gap <50 μm) and no micromotion (<30 - 150 μm, over which leads to fibrous ingrowth which is painful and unstable).
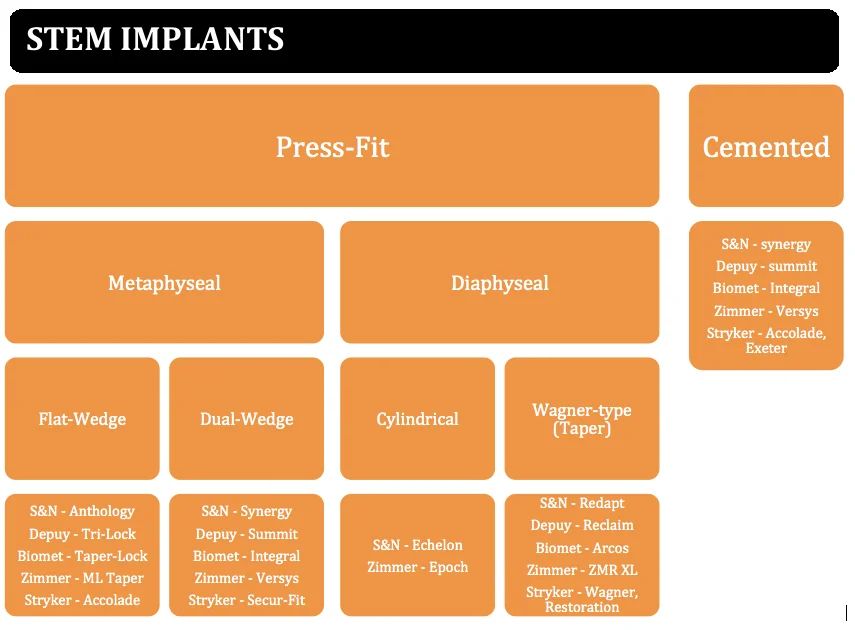
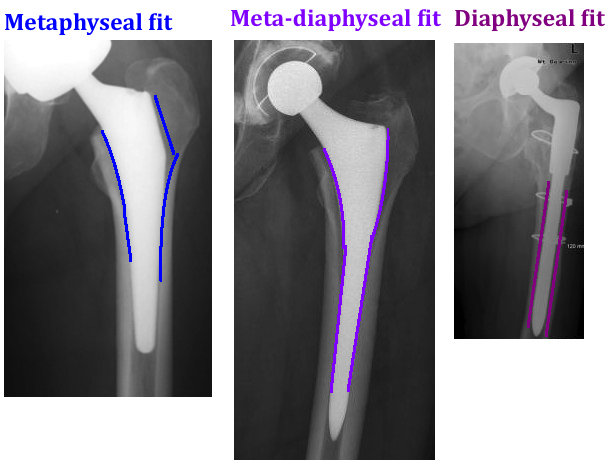
Press-fit can occur at the 1) metaphysis (the standard for primary hip replacements), or it can occur at the 2) meta-diaphysis (when someone is very osteoporotic and the surgeon is not sure if they can rely purely on the softer metaphyseal bone for rigid fixation) or it can occur at the 3) diaphysis (the standard for revision hip replacements, when the metaphyseal bone is gone).
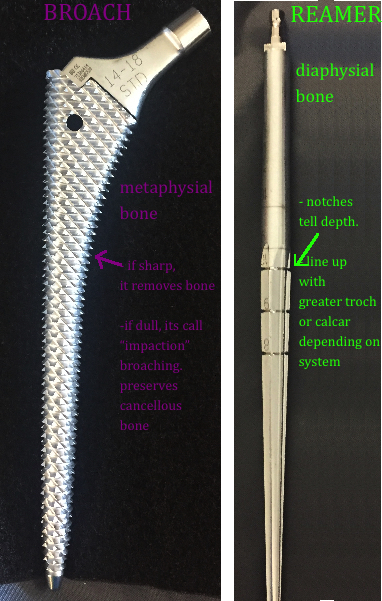
The technique to prepare the femoral canal for the stem implant utilizes broaching alone for the metaphyseal fitting stems, and utilizes reaming for the meta-diaphysial and diaphysial fitting stems. Broaching prepares the metaphysis, while reaming prepares the diaphysis.
The stem is designed so that it is slightly larger than the femoral canal that was prepared through sequential broaching, and by wedging in a slightly "oversized" stem, the hoop stress prevent motion.
The alternative is "line-to-line" preparation of the femoral canal, the canal and the stem are a perfect match in size, however, the rough coating of the stem creates enough friction to prevent motion (aka "scratch fit" or "interference fit").
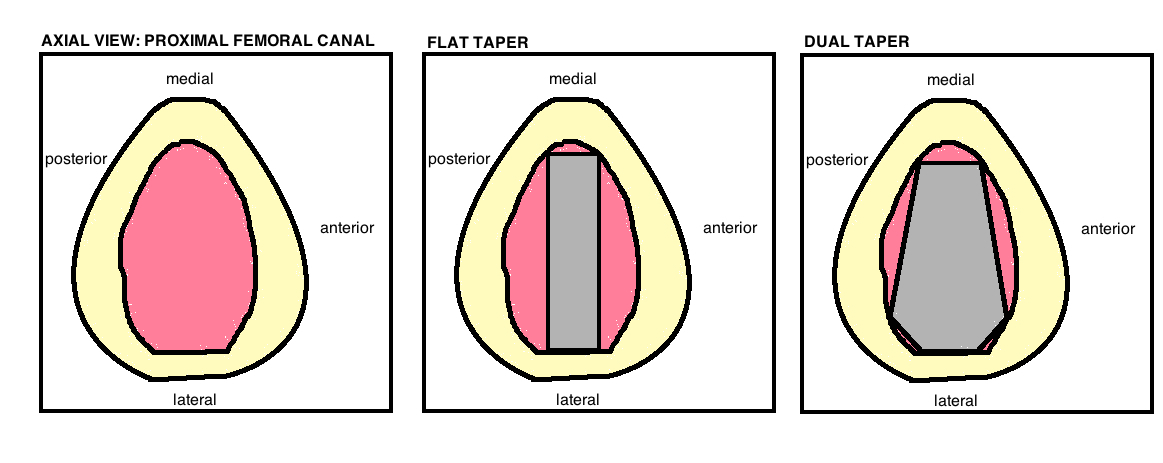
The variability of femoral canals (ie Dorr Classification) prevents a single stem design from truly standing out. The design type determines the area of the femoral canal where fixation occurs and the surgical technique required for implantation.
2. biologic fixation is the mid-term goal.
The goal is for bone to incorporate into the implant. Therefore, the implants are typically titanium alloy so the implant modulus of elasticity is the closest match to bone. There is either bony ingrowth or bony ongrowth. Bone growth is circumferential to prevent communication between the joint space and the distal aspect of the component (which is called a large "effective joint space" and can occur when there is incomplete proximal coating).
Bone ingrowth occurs with porous coating, achieved by heating the metal (which can decrease the fatigue strength). The optimal pore size is between 50 - 150 μm), the deeper the pores, the better the ingrowth, and overall porosity 40 - 50%.
Bone ongrowth occurs with a “roughened” surface (divots not pores). This roughened surface occurs by grit blasting (a pressurized spray of aluminum oxide particles to produce an irregular surface at 3-8 μm depth, this depth = the "roughness" and greater roughness = greater fixation). Plasma spray (applying molten metal in a argon gas environment) also creates roughened surface. The depth of pores and depth of divots are both directly proportional to strength of fixation. Because pores are deeper than divots, its clear that ingrowth gives better fixation than ongrowth per mm^2. To compensate, the surface area of bone ongrowth must be greater (and its used almost only for stems, not cups). Furthermore, the Bone ongrowth technique requires press-fit technique (cannot use scratch fit).
note: bone ongrowth can also occur with stems containing splines (longitudinal grooves that travel along the diaphyseal portion of the stem)
Hydroxyapatite coating is an osteoconductive calcium phosphate coating applied by plasma spray. It is shortens the time to biologic fixation.
3. BALANCED STRESS distribution across the femur is the long-term goal of cementless stems.
The key to longevity is equal distribution of stress across the prosthesis.
Uneven stress causes “stress shielding” the areas that do not experience stress. Stress shielding is the resorption of bone over time because the bone is not functioning in its normal capacity, and thus answers in the affirmative to the question: “is it true that if you don’t use it, you lose it?” In contrast, areas that experience excess stress are painful and prevent bone ingrowth. Titanium alloy is preferred because its lower modulus of elasticity is most compatible with cortical bone (shares the stress) thus decreasing thigh pain (yet one study [26] compared identical design stem in titanium and cobalt-chrome and showed all thigh pain and stress shield was only related to larger stem size because the radius is such a powerful determinant of rigidity, remember its r4).
GEOMETRY OF STEMS
Multiple designs attempt to achieve the aforementioned 3 Goals of uncemented hip arthroplasty.
Flat Tapered, "Single-Wedge", "Blade". This design refers to an approach for achieving early fixation by wedging a rectangle into a circular hole. The intentional mismatch of geometry achieves good torsional stability. Fixation occurs by medial-lateral engagement and by the 3-point fixation along the length of the stem. Its broach only. There is no reaming because there isnt significant distal engagement as the stem tapers in the medial-lateral plane. The minimal distal contact between implant and diaphysis helps to prevent proximal bone resorption (known as "disuse osteopenia" or "stress shielding" which is an issue with the cylindrical stems that engage the diaphysis). The stem often has a recessed shoulder to reduce the need to resect bone laterally.
Every implant company makes a stem with this design. Smith & Nephew: Anthology, DePuy: Tri-lock , Stryker: Accolade II , Biomet: Taperlock, Zimmer: M/L Taper.
Dual Taper, "Elliptical". This design refers to an approach for achieving early fixation by completely filling the metaphyseal canal and circumferentially engages the femoral cortex proximally. The technique is often referred to a "Fit-n'-Fill" technique requiring both reaming and broaching. The implant tapers in all planes and is overall more substantial in volume as compared to a single-wedge design.
These designs are usually made for cementless and cemented option. Every implant company makes a stem with this design. Smith & Nephew – Synergy; DePuy – Summit;Stryker - Secur-Fit, Biomet - Integral, Zimmer - Versys.
Cylindrical. This design refers to an approach for achieving early fixation by engaging not only the metaphysis but also the diaphysis for ingrowth. The cylindrical model engages the diaphysis because there is no taper (unlike the aforementioned examples). It was developed to address patients with poor metaphyseal bone quality that put them at risk for failure to achieve initial stability or later ingrowth. The disadvantage of the stems is that ingrowth is rarely uniform across the entire stem, and the majority occurs distally, which then assumes the majority of the stress leading to "stress shielding" in the proximal metaphysis, which leads to significant bone loss. This design is used for primaries, although it has been replaced by the two aforementioned designs in most centers. This design is rather preferred for revision surgery.
Most implant companies make a stem with this design. Smith & Nephew - Echelon, DePuy – AML, Solution , Stryker - Secur-Fit Max, Biomet – Mallory-Head, Zimmer - Epoch
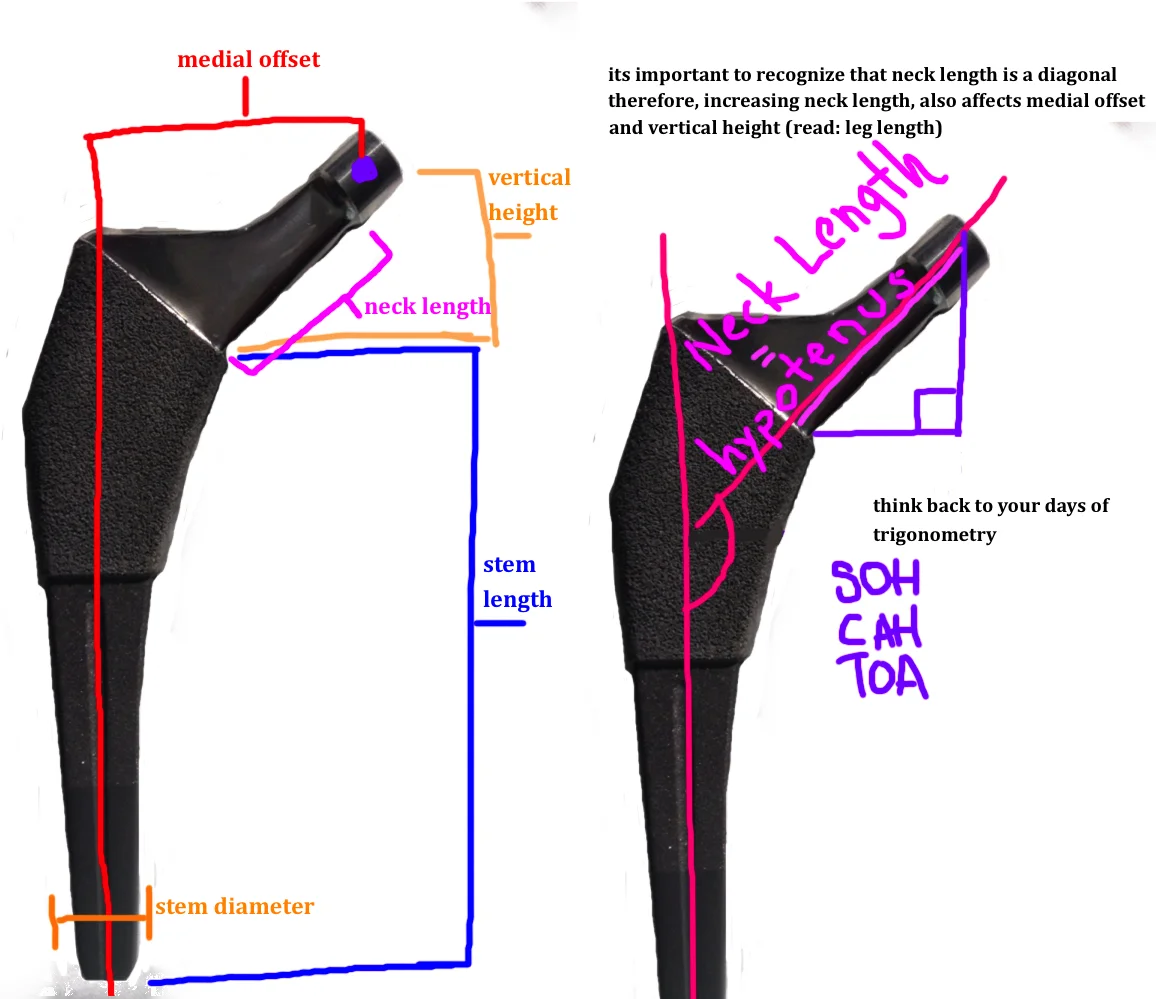
Wagner-Type. This design refers to an approach for achieving early fixation by engaging the diaphysis for ingrowth. The Wagner-type design is a tapered cylinder (axial stability) with splines to grip the cortex circumferentially (rotational stability). The initial design was monoblock (stem is one unit), however, many of the popular current designs are "Modular", meaning there are two parts to the stem that allows the surgery to adjust stem height once the diaphyseal portion has been implanted. A Modular Stem is beneficial for a few reasons. For one, you can adjust the degree of anteversion to help reduce dislocation risk. Additionally, because these stems are often used in the face of significant bone loss, there is some subsidence of the stem when its inserted (meaning: the line you use to measure depth when you are reaming the femoral canal does not always equal the height of the actual stem once its inserted). Some of this depends on the steepness of the taper. A 1 degree taper is a shallow transition and may subside more than a 3 degree taper, which is sharper and thus prevents some subsidence. The standard taper is a 2 degree, which some variation between companies.
Most implant companies makes a stem with this design. Smith & Nephew - Redapt, DePuy - Reclaim, Stryker - Restoration, Biomet - Arcos , Zimmer - ZMR or Wagner SL.
Bone Preserving. This design refers to an approach for metaphysial for ingrowth that attempts to preserve bone by performing a high femoral neck cut. The implant is smaller than a standard flat taper stem, and looks like a small "chili pepper", but obtains fixation similar to the single wedge taper design that relies on 3-point fixation. There is greater variability in the femoral neck person to person than in other areas of the proximal femur. Therefore, the problem with this design is that multiple iterations of one stem (varus, valgus, etc) are needed to account for these variations.
Some implant companies makes a stem with this design. Zimmer - Fitmore, Biomet - Microplasty.