Placement of the acetabular component depends on the appropriate version, inclination, depth, and height.
The goal of cup placement is to match the implant's range of motion to the native hip's range of motion. When these two overlap, there is no impingement which means the cup is in a "safe zone".
Impingement occurs when our anatomy wants to move the hip beyond what is permitted by the orientation of the implant. For example, the architecture of our body is designed to allow the femur to adduct about 30 degrees, however, if the cup is not properly anteverted, neck of the implant will impinge on the cup at only 20 degrees. And if impingement occurs, its like a car hitting a brick wall: motion comes to a halt, and the implant can either lever out (dislocate), or generate wear particles at an accelerated rate.
We will review the primary considerations for cup placement.
1. Version
Version is the orientation of the implants in the sagittal plane. Neutral version means the cup is facing completely lateral, ie completely in line in the sagittal plane. Anteversion means the cup is facing slightly anteriorly, this allows for increased hip AD-duction. In contrast, Retroversion means the cup is opening up slightly posteriorly. This allows for increased hip AB-duction, but less adduction, and if the hip moves into too much adduction it will impinge on the rim of the cup.
The target Acetabular Cup version is slight Anteversion. There is a “safe zone” between 5° and 25° (ie 15° +/- 10°) to match native hip motion and avoid impingement [2, 3]. It can be assessed postoperatively by cross leg lateral XR (a frog-leg lateral gives lateral view of femur, but an AP of the acetabulum).
There is also Femoral Stem version. The stem should also be angled slightly forward (anterior), about 15°. The goal of Combined Anteversion is 35° (+/- 10°) [4]. Studies demonstrate that maximal range of motion before impingement occurs when the acetabular components are placed within this “safe-zone” [5, 6]... which corresponds to the the native acetabular positioning within the pelvis.
True version of pelvis is angle between a) the line from the posterior to anterior wall of acetabulum (essentially the ilioischial line) and b) a line directly from A to P (this is the alpha angle). A CT scan gives the best picture of version.
The expectation for hip ROM after THA is 110 ° flexion and 30 ° extension. Increasing the acetabular anteversion increases the flexion (decreases extension).
2. Inclination
Inclination is the orientation of the cup in the coronal plane.
The target acetabular cup inclination is a "safe zone" between 30-50° abduction (assessed by AP of hip).
Excessive inclination (a vertically oriented cup) decreases the surface area of articulation along the superior dome of the cup and therefore increases contact forces causing higher wear rates (known as edge loading). Insufficient inclination (a horizontal cup) decreases range of motion (risks impingement with hip abduction), but is generally considered less problematic than too much inclination.
3. Depth
Target is to recreate the anatomic hip center for that patient by reaming to bleeding cancellous bone (assessed by AP of hip: cup should be up to, but not past Kohler’s line, aka ilioischial line).
Over medializing the cup removes excess bone (always preserve bone, “A.P.B”, is a mantra for TJA surgeons). However, failure to sufficiently medialize the cup provides less surface area for bony ingrowth, and the cup does not reach the bleeding cancellous bone that promotes ingrowth. Lastly, recall the force diagram showing the two opposing lever arms converging at the hip center…a lateralized hip center shortens the “abductor lever arm” and thus requires the abductors to work harder to counteract the body weight force acting on the hip.
4. Height.
Inferior border of cup should be at the “tear drop” , assessed by AP of hip.
Clinical Correlate: A high hip center (which is sometimes done intentionally in cases of DDH when there is poor native bone stock around the native acetabulum) affects the abductor muscle tension and increases the joint reactive forces.
5. Pelvic Tilt
Acetabular orientation is not fixed. There is a dynamic relationship between the pelvis and the lumbosacral spine, which moves in a predictable way, from standing to sitting, to maintain sagittal balance.
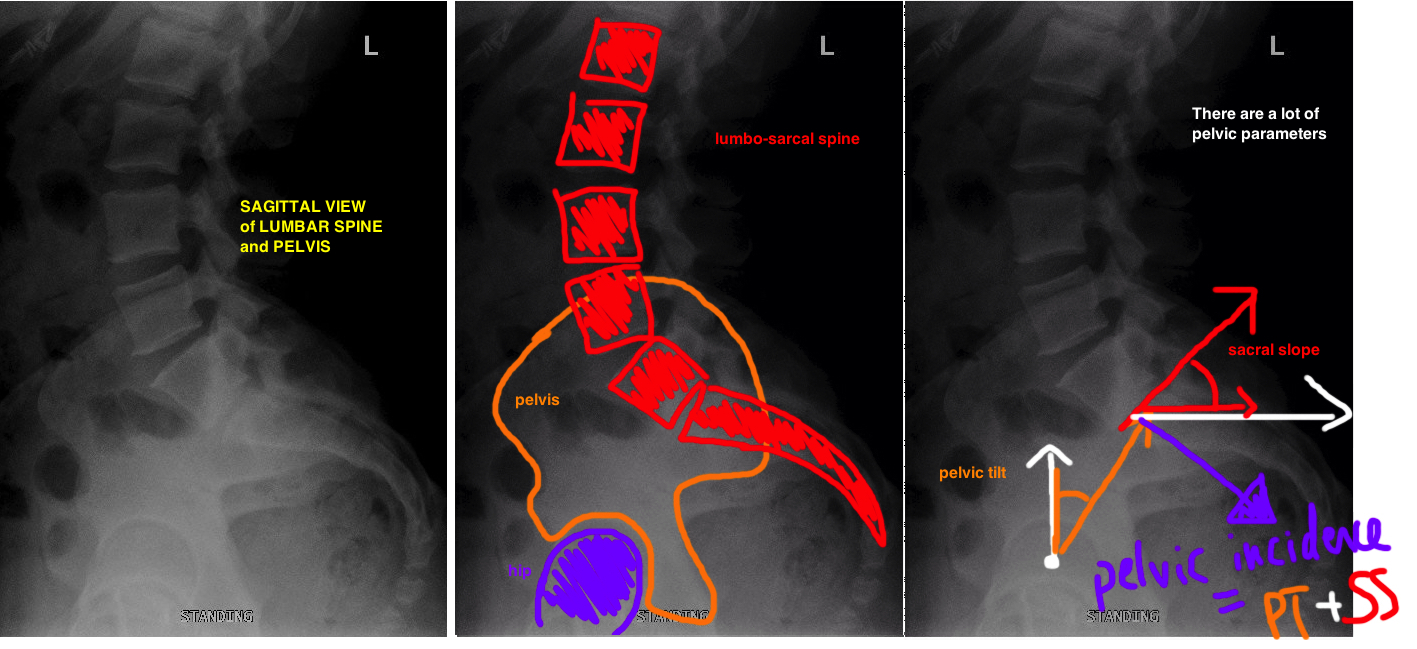
The basic concept is that pelvic tilt and sacral slope are dynamic pelvic parameters (change with body position), but their sum represents the Pelvic Incidence, which is static (always the same number regardless of position).
The Pelvic Incidence is a fixed number in adults, it represents overall body balance. Yet as we move into different positions (sitting, standing, lying down), the SS and PT change in order to maintain PI.
When standing, the amount of lumbar lordosis increases (SS increases), so the pelvis tilts forward, ie flexes (represented as a decreasing PT).
During sitting, the Pelvis Tilts backwards (ie extends) causing increased PT. Increasing Pelvic Tilt Increases Acetabular Anteversion (at a rate of 1.0° pelvic tilt to 0.7° of anteversion) [6]. Increasing the anteversion prevents anterior impingement (its important to avoid anterior impingement bc it causes the femoral head to lever out posteriorly). During sitting the lumbar lordosis decreases (SS decreases).
The SS and PT change by the same amount in a normal flexible spine-sacrum to maintain the PI (balance). Sitting after THA risks posterior dislocation because of anterior impingement, therefore, a mobile lumbo-pelvic segment is essential to minimizing THA dislocation. However, Lumbar Fusion reduces lumbo-pelvic motion and risks THA dislocation. The more lumbar segments fused, the less lumbo-pelvic flexibility and the higher the dislocation risk: No fusion: 1.5% risk. 1-2 levels: 2.7% risk. 3-7 levels: 4.6% risk [7, 8].
Lets look more at the measurements to describe the orientation of pelvis [9].
Pelvic incidence (PI) is the main axis of sagittal balance of the spine (ranges 48° - 53° ). It is the angle between Line 1 (perpendicular to Sacral Prominotry, aka superior plate of S1) and Line 2 (center of Sacral prominitory to Hip Center)
Sacral slope (SS) is the angle of the sacrum. Angle between Line 1 (line parallel to sacral prominotry) and Line 2 (a horizontal reference line)
Pelvic Tilt (PT) is the angle of the pelvis. Angle btwn Line 1 (center of Sacral prominitory to Hip center) and Line 2 (a vertical reference line). As the upper pelvis moves posterior, the pelvic tilt increases, therefore pelvic tilt can be thought of as the degree of pelvic extension. When the upper pelvis tilts forward (anterior flexion), there is less pelvic tilt. Pelvic tilt does not change after THA. With normal saggital balance (PI), the PT should be < 22°.
REFERENCES
1. Lewinnek, G.E., et al., Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am, 1978. 60(2): p. 217-20.
2. Biedermann, R., et al., Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation of the acetabular component. J Bone Joint Surg Br, 2005. 87(6): p. 762-9.
3. Dorr, L.D., et al., Combined anteversion technique for total hip arthroplasty. Clin Orthop Relat Res, 2009. 467(1): p. 119-27.
4. Kosashvili, Y., et al., Acetabular alignment and primary arc of motion for minus, skirtless, and skirted 28-, 32-, 36-, and 40-mm femoral heads. J Arthroplasty, 2013. 28(2): p. 279-285 e2.
5. D'Lima, D.D., et al., The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am, 2000. 82(3): p. 315-21.
6. Lembeck, B., et al., Pelvic tilt makes acetabular cup navigation inaccurate. Acta Orthop, 2005. 76(4): p. 517-23.
7. Perfetti, D.C., et al., Prosthetic Dislocation and Revision After Primary Total Hip Arthroplasty in Lumbar Fusion Patients: A Propensity Score Matched-Pair Analysis. J Arthroplasty, 2016.
8. DelSole, E.M., et al., Total Hip Arthroplasty in the Spinal Deformity Population: Does Degree of Sagittal Deformity Affect Rates of Safe Zone Placement, Instability, or Revision? J Arthroplasty, 2016.
9. Phan, D., S.S. Bederman, and R. Schwarzkopf, The influence of sagittal spinal deformity on anteversion of the acetabular component in total hip arthroplasty. Bone Joint J, 2015. 97-B(8): p. 1017-23.