Instability is the 2nd leading cause of THA revision (22% of revisions nationally [1]) and remains a notable problem despite some implant advances, such as dual mobility cups. The risk of dislocation in primary THA is roughly 1% at 1 month, 2% at 1 year, then an additional 1% every 5 years (7% at 25 years). [2, 3] . The risk of dislocation in revision THA is significantly higher: 5-7% within the first year.
Risk factors are both Patient-based and Surgical-based.
▪ Patient based risk factors include females, prior hip surgery (2x increased risk), neuromuscular disease, inability to comply with hip pre-cautions such as alcohol abuse (4x increased risk) and cognitive impairment (such as dementia), older age (especially those over 80 years old), and THA for treatment of osteonecrosis or acute femoral neck fracture (the idea being that an acute need for hip arthroplasty does not give the capsule and surrounding tissue time to thicken and act as a strong soft tissue support as seen in gradual osteoarthritis progression). [4] [5]
▪ Surgical based risk factors relate to the approach (controversial) as well as the components and their positioning (also controversial).
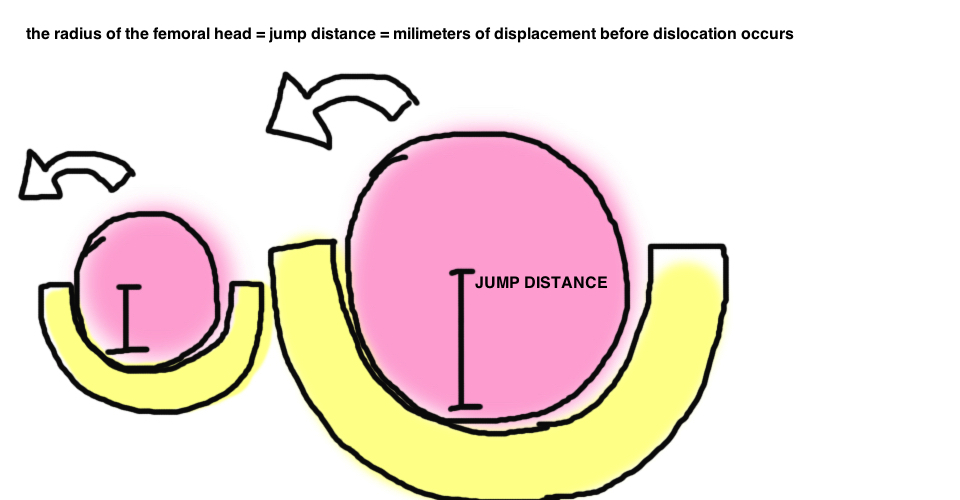
Femoral head size.
Remember that larger head size increases both jump distance and arc before motion before impingement and therefore, in theory, decreases dislocation risk. In general, the rate of dislocation from primary THA is steadily declining since the 90s, and this correlates with the gradual increase in average femoral head size. Furthermore, one study demonstrated that larger femoral heads were associated with lower dislocations, particularly when using the posterolateral approach (with a 12% dislocation risk in 22-mm heads at 10 years vs. 6.9% for 28-mm heads vs. 3.8% for 32-mm heads [2]). The benefit of increasing femoral head size to treat instability during revision THA has also been demonstrated [6] [7]. Both the combined theoretic and academic evidence supports the correlation between increased femoral head size and stability.
Yet a larger head size is not all sunshine and theres no free lunch in medicine. Although highly cross-linked poly doesn’t appear to generate greater volumetric wear with larger head sizes [8]…there does appear to be a correlation between femoral head size and torque at the head-neck trunion, with risk of increased metal debris. Additionally, larger head size requires larger cup size, which in turn requires greater acetabular bone resection (some studies promoting larger heads utilized thinner metal cups as the bone-conserving solution, yet these metal-on-metal implants have since fallen out of favor).
Component Positioning.
The components must be positioned so that implant arc of motion mirrors the native hip’s functional arc of motion. The classic paper by Lewinnek describes the safe-zone of component positioning: Cup inclination 40° ± 10°, Combined Cup-Stem anteversion 35° ± 10° (see basic concepts) [9]. In theory, this safe zone maximizes hip range of motion before impingement occurs (impingement causes the femoral head to lever out of the joint). However, studies comparing component positioning in stable vs. dislocated hips have shown no overall difference in component placement [10, 11]. While its agreed that a general adherence to standard cup version and inclincation is important to prevent dislocation, these studies demonstrate that positioning is not the only variable at work, and patient related factors have a big impact on stability, and the true “safe zone” may not be the same for all patients. The role of pelvic tilt has become integral to this conversation of a “physiologic safe zone”.
Soft Tissue Envelope.
Dislocation rates for the posterior approach decrease dramatically when the soft tissue is repaired. Furthermore, many argue that the Anterolateral and Direct Anterior improve hip stability by preserving soft tissue. The Abductor Complex remains the most important soft tissue restraint to dislocation. The Abductor complex pulls the head into the socket, and its absence leads to instability that is the hardest to control. Increasing the hip offset places greater tension on the abductors and can increase stability. A greater trochanteric advancement, performed by Charnley in all his THA, increases tension on the abductor complex by moving its insertion point distally.
In the revision setting, fracture of the greater trochanter can lead to “troch escape” whereby the entire abductor complex insertion migrates proximally taking tension off the muscle and causing both a Trendelenberg gait and hip instability.
Surgical Approach.
The effect of surgical approach on risk for instability remains controversial. The importance of the soft tissue envelop for stability is well recognized. The posterior approach without soft tissue repair has the highest rate of dislocation (between 4-9%, which is 6-8x higher than an anterolateral approach, “Watson-Jones”), however, with meticulous soft tissue repair, dislocation rates approach to levels comparable to other surgical approaches [12]. One study showed that components were 3x more likely to be within the safe zone in a posterior approach, and yet there remained a significantly higher dislocation rate [10]. This presents an interesting contrast with regard to these 2 important variables for hip stability. One may argue that great emphasis is placed on component positioning, because this is something that surgeons can control and can measure postoperatively. Yet increasing evidence highlights the greater importance of soft tissue in preserving hip stability. The Direct Anterior approach (“Smith-Peterson”) may have a lower risk of dislocation compared to posterior, but this remains controversial [13] [14] [15]. The DA preserves soft tissue and avoids abductor release, which likely promotes greater stability (although it is associated with higher rates of intraoperative femur fracture). The role of hip precautions in with the DA approach is not required, suggesting increased stability due to less soft tissue injury [16].
Outcomes.
The timing of dislocation relative to the index procedure is important. The majority occur in the first 4-6 weeks (60%) and the prognosis is better with earlier dislocations, with an 33% risk of further dislocation. In comparison, dislocations occurring after 6 weeks postop (called a “late dislocation”) have a 55% recurrence risk. [17]
Treatment.
Most 1st time dislocations are managed nonoperatively with the goal of limiting hip flex to 40°, maintainat least 10° abduction, and prevent internal rotation. While theres no good evidence to suggest that a brace reduces dislocation rates, they may have some benefit in reminding some patients to be mindful and can thus be worn for 4-6 weeks after dislocation[18]. Many surgeons abide by the three strikes and your out rule; meaning surgical intervention is required if the hip dislocates more than 3 times. Planning for surgery requires looking at leg lengths, offset, the abductor strength, and implant position (a CT to best evaluate version if thats a concern [19]).
Operative options depends on the problem, but always remember that instability is main complication following revision surgery, so it can be easy to get caught chasing your tail if your not effective at identifying and solving the problem.
If the components are well positioned, then look for soft tissue insufficiency. A larger femoral head can increase jump distance, or an elevated rim can provide a buttress to prevent posterior dislocation (but it risks component impingement and dislocation in the countercoup direction). Increasing offset can help by placing abductors under greater tension. This can be achieved through an offset liner, or by changing the femoral component to a High Offset neck (which has a neck angle of 115°, as compared to 125-135° in a standard neck, which increases the abductor lever arm but also affects leg lengths). A trochanteric advancement similarly places the abductors under greater tension, but has notable complications (troch escape syndrome).
A more severe abductor deficiency (which should be evaluated with Trendelenburg Test, and EMG) may require a constrained liner for low demand patients…low demand is key because the constraint decreases joint motion and transfers increased force to the component-bone interface and thus increases loosening rates). Dual mobility cups also provide stability for severe abductor deficiency, and have promising results, particularly in the more active population (although there is concern for higher rates of debris generation with the two articulations).
REFERENCES
1. Bozic, K.J., et al., The epidemiology of revision total hip arthroplasty in the United States. J Bone Joint Surg Am, 2009. 91(1): p. 128-33.
2. Berry, D.J., et al., Effect of femoral head diameter and operative approach on risk of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am, 2005. 87(11): p. 2456-63.
3. Berry, D.J., et al., The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am, 2004. 86-A(1): p. 9-14.
4. Paterno, S.A., P.F. Lachiewicz, and S.S. Kelley, The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am, 1997. 79(8): p. 1202-10.
5. Woolson, S.T. and Z.O. Rahimtoola, Risk factors for dislocation during the first 3 months after primary total hip replacement. J Arthroplasty, 1999. 14(6): p. 662-8.
6. Sikes, C.V., et al., Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty, 2008. 23(7 Suppl): p. 59-63.
7. Amstutz, H.C., M.J. Le Duff, and P.E. Beaule, Prevention and treatment of dislocation after total hip replacement using large diameter balls. Clin Orthop Relat Res, 2004(429): p. 108-16.
8. Lachiewicz, P.F., et al., Femoral head size and wear of highly cross-linked polyethylene at 5 to 8 years. Clin Orthop Relat Res, 2009. 467(12): p. 3290-6.
9. Lewinnek, G.E., et al., Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am, 1978. 60(2): p. 217-20.
10. Abdel, M.P., et al., What Safe Zone? The Vast Majority of Dislocated THAs Are Within the Lewinnek Safe Zone for Acetabular Component Position. Clin Orthop Relat Res, 2016. 474(2): p. 386-91.
11. Esposito, C.I., et al., Cup position alone does not predict risk of dislocation after hip arthroplasty. J Arthroplasty, 2015. 30(1): p. 109-13.
12. Kwon, M.S., et al., Does surgical approach affect total hip arthroplasty dislocation rates? Clin Orthop Relat Res, 2006. 447: p. 34-8.
13. Sheth, D., et al., Anterior and Anterolateral Approaches for THA Are Associated With Lower Dislocation Risk Without Higher Revision Risk. Clin Orthop Relat Res, 2015. 473(11): p. 3401-8.
14. Barnett, S.L., et al., Is the Anterior Approach Safe? Early Complication Rate Associated with 5090 Consecutive Primary Total Hip Arthroplasty Procedures Performed Using the Anterior Approach. J Arthroplasty, 2015.
15. Berend, K.R., et al., Primary and revision anterior supine total hip arthroplasty: an analysis of complications and reoperations. Instr Course Lect, 2013. 62: p. 251-63.
16. Restrepo, C., et al., Hip dislocation: are hip precautions necessary in anterior approaches? Clin Orthop Relat Res, 2011. 469(2): p. 417-22.
17. von Knoch, M., et al., Late dislocation after total hip arthroplasty. J Bone Joint Surg Am, 2002. 84-A(11): p. 1949-53.
18. Dewal, H., et al., Efficacy of abduction bracing in the management of total hip arthroplasty dislocation. J Arthroplasty, 2004. 19(6): p. 733-8.
19. Pierchon, F., et al., Causes of dislocation of total hip arthroplasty. CT study of component alignment. J Bone Joint Surg Br, 1994. 76(1): p. 45-8.