The Knee is more complex than a simple hinge joint. Motion occurs not only in flexion-extension, but also involves rotation, pivot, and gliding movements. The best way to understand our knee motion is to first understand that it is controlled by three things: 1) the articular geometry; 2) the ligamentous balance; and 3) muscular tension. We will look at these individually to appreciate the complexity of knee kinematics.
1. The Articular Geometry.
Lets first look at the femoral side of the joint.
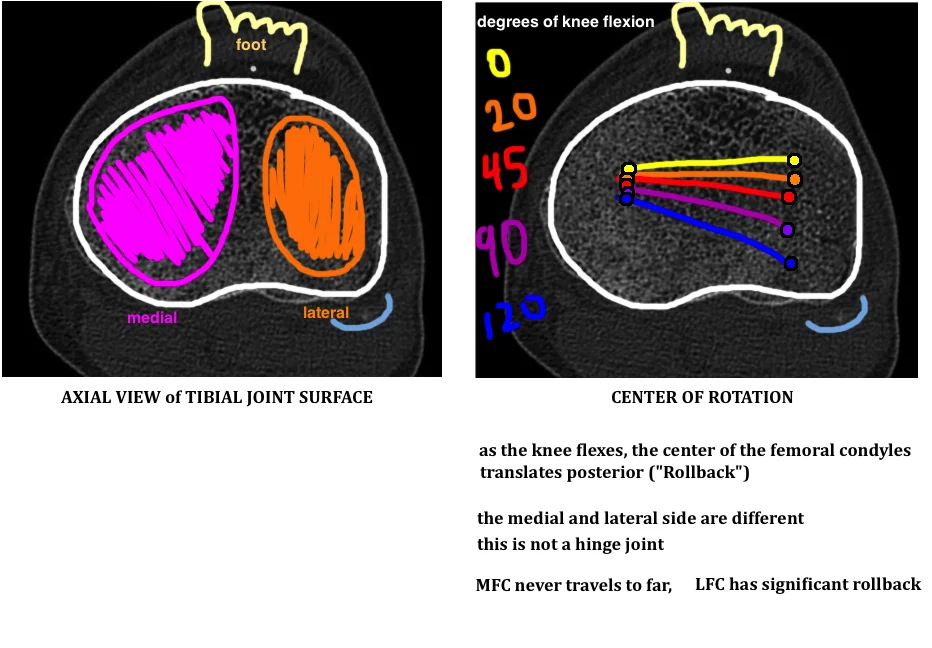
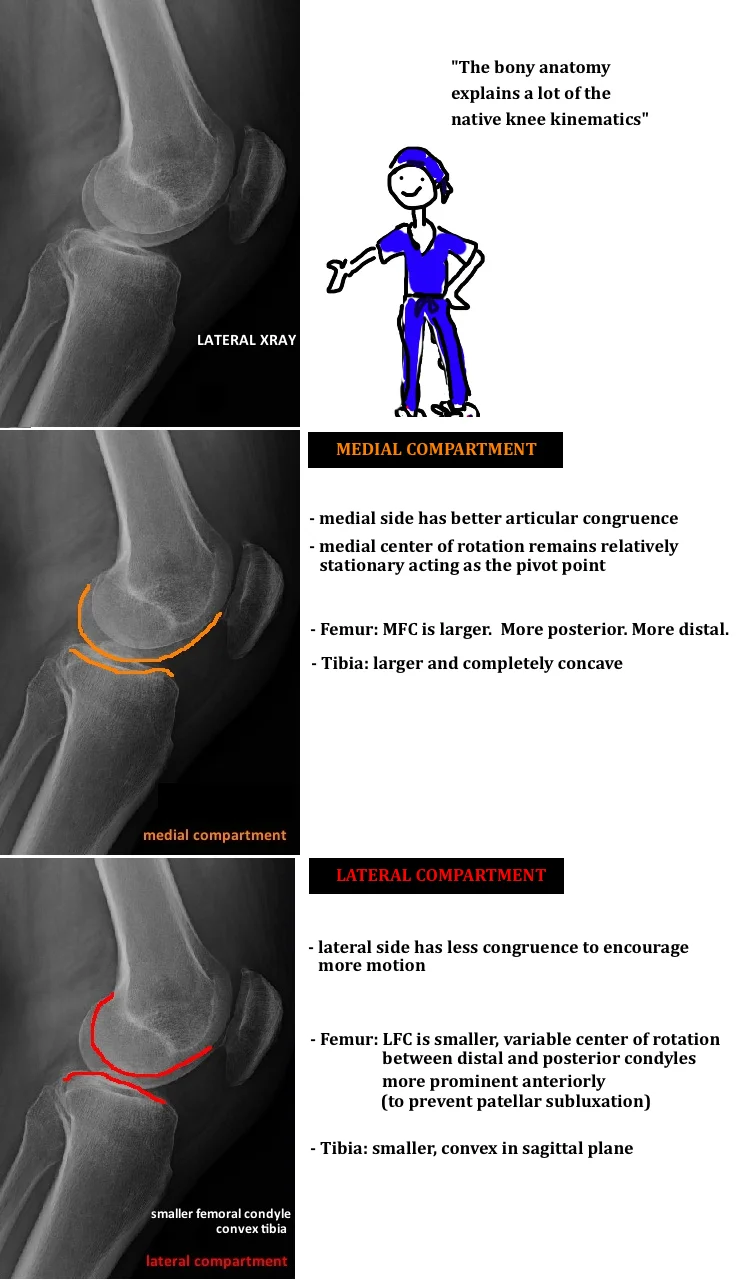
The medial femoral condyle (MFC) and lateral femoral condyle (LFC) are different sizes and have a different radius of curvature. The MFC is larger and more circular – meaning a uniform radius of curvature. In contrast, the LFC is smaller and the two condyles, distal condyle and posterior condyle, have very different radii of curvature to promotes LFC motion during knee flexion.
The differences in femoral anatomy create unique motion patterns for the MFC and LFC and this drives complex kinematics. For example, the MFC radius of curvature is relatively uniform and so the MFC remains mostly stationary during knee flexion, while the LFC travels posteriorly on the tibia (posterior rollback) due to the change in radius of curvature.
The difference in posterior rollback between the LFC and MFC (LFC rolls back while the MFC remains relatively in place) drives the distal femur to externally rotate. The majority of this external rotation occurs in the first 15° of knee flexion. This contributes to patellar tracking because at 15° of knee flexion the patella engages the trochlear groove and this is the stress point where the patella needs to be centrally located to prevent lateral dislocation or subluxation. Patellar maltracking can occur if the femur doesn’t rotate or if there is insufficient medial structures (specifically the medial patellofemoral ligament) acting as a harness to guide the patella, or a hypoplastic trochlear groove can also lead to patellar subluxation by failing to provide a bumper to guide tracking. So as the femur flexes, it externally rotates about 15° in relation to the tibia and thus the trochlear groove moves a little laterally to help with patellar tracking.
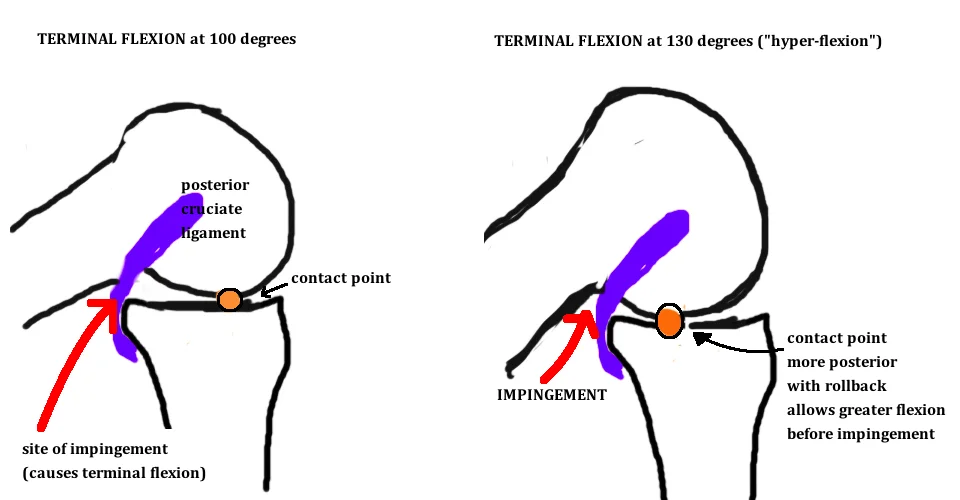
Posterior rollback is a big deal for another reason. It determines the point of terminal flexion. In many ways it’s the holy grail of TKA. Rollback is essential to achieve full deep flexion (which is seen with squatting or deep bends). Without rollback, the back of the femoral diaphysis will impinge on the tibia around 90°, however, if the distal femur moves posteriorly in relation to the tibia, it increases the clearance before impingment, and thus allows for extra flexion. Ultimately, impingement does occur (between the lateral tibia and the posterior cortex of the distal femur) and this marks terminal flexion. We talk more about the importance of rollback when discussing TKA designs (see link).
The medial and lateral tibial plateau are also shaped differently. The difference in the medial and lateral tibia is best seen on a lateral x-ray of the knee (or in comparing slices of a CT scan). The lateral tibial plateau is flat (or even slightly convex) and is designed this way to encourage LFC roll back during knee flexion. In contrast the medial tibial plateau is dished (concave), allowing for less MFC rollback, and enabling a pivot type motion whereby the LFC rotates around the stable MFC.
2. Ligament STABILIZATION
The knee is only partially guided by the geometry of the articular surface. The surrounding ligaments and muscles also play a central roll.
Collateral Ligaments: control coronal plane stability.
The superficial MCL is the major medial stabilizer, originating at the medial epicondyle and traveling deep to the pes muscles to insert broadly on the tibial 4.5 cm distal to the joint line. The deep MCL is only a thickening of the capsule (as known as the medial capsular ligament). The posterior-medial corner (posterior oblique ligament, semimembranosus, posterior horn medial meniscus) provide 30% of valgus restraint in full extension and with greater flexion the MCL assumes more responsibility - 60% in 5° flexion and 80% in 25° flexion.
The LCL ("fibular collateral ligament") provides lateral stability, originating proximal and posterior to the lateral epicondyle and inserts on the lateral fibular head.
Cruciate Ligaments: provide stability in the sagittal plane.
The anterior cruciate ligament (ACL) prevents anterior subluxation of the tibia, particularly near terminal extension - ACL is taut around 15° of flexion, which corresponds to the region where your quad has the worst mechanical advantage to extend the leg, and thus exerts the greatest anterior directed force on the proximal tibia. In ACL-deficient knee, full extension causes the femur to shifted posteriorly due to un-resisted anterior pull on the tibia.
ACL function changes the location of cartilage wear. Wear occurs in the anterior-medial aspect of the knee when the ACL is intact, however if the ACL is deficient, the tibia translates forward, and cartilage wear occurs in the posterior-medial aspect of the knee. Its important to recognize wear-pattern differences when considering UKA.
In contrast the posterior cruciate ligament prevents posterior subluxation of the tibia. If the tibia subluxes posteriorly, the femur is unable to achieve proper posterior rollback, which is essential for achieving terminal flexion. We discuss in the Knee Design Section the importance of the PCL for TKA.
Meniscus: increase contact area to reduce joint forces
The menisci improve joint congruity by smoothing out the difference between relatively round femoral condyles and flat tibial plateaus. The menisci increase the effective joint surface (a complete meniscectomy reduces the contact area by 50%), which reduces contact forces. Menisci transmit 50% of the load in extension and 90% in flexion by transferring axial load into hoop stress. Complete meniscectomy increases joint forces by 2-3x, with 20% of people developing significant arthritis in just 3 years, and 100% of people develop significant arthritis by 20 years.
The medial meniscus is relatively stationary, similar to the MFC, and the posterior horn of the medial meniscus can act as an A-to-P stabilizer, and is particular important where the ACL is absent. Over time, the posterior horn of the medial meniscus becomes degenerated in people without an ACL.
3. Muscles
The muscles contribute to knee motion.
The Quad is the knee extensor and weakness/atrophy affects patellar tracking and is associated with patellofemoral pain.
The Popliteus "unlocks" the knee as it begins to flex. In full extension there is close articular congruency, however, as the knee enters flexion, the popliteus muscle externally rotates the femur relative to the tibia, to decrease articular congruence and to enable normal condylar rollback and full flexion. It is a posterior muscle, that crosses the knee from the medial tibia to the lateral femur, the tendonous portion becomes intraarticular, runs just behind the lateral meniscus, and inserts at the lateral femoral condyle (anterior and distal to the epicondyle).