We now apply the understanding knee alignment to make our bone cuts.
In this discussion, to explain the goal of each cut in the simplest manner, we will be talking about the "Measured Resection" technique of making bone cuts to achieve "Mechanical Alignment". There is also a "Gap Balancing" technique to bone cuts (the difference is discussed here).
1. Tibial cut.
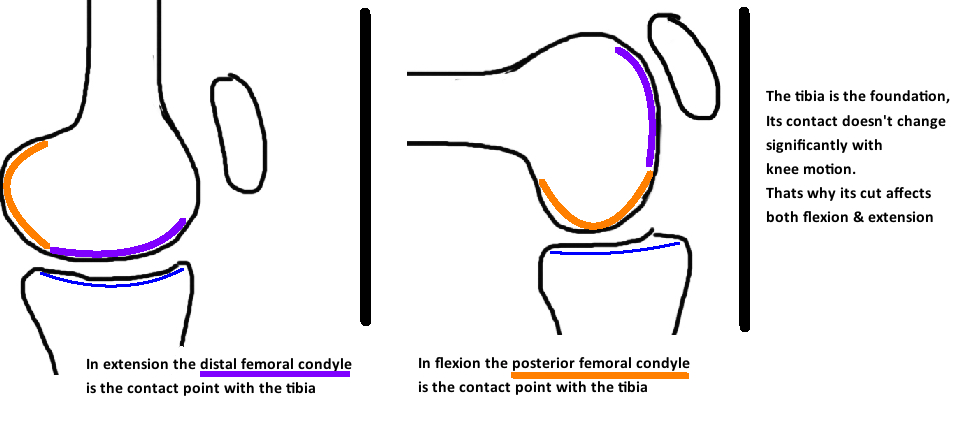
The tibial cut is aimed at 0 degrees (perpendicular to the mechanical axis). The tibial cut is arguably the most important bone cut in TKA because it affects both the Flexion and Extension gap. Think of it as the foundation upon which you build the TKA. The tibia affects both the Flexion and Extension gap because it articulates with the Distal Femoral Condyles in Extension, and the Posterior femoral condyles in Flexion. Contact Point changes significantly for the femur during the knee arc of motion, it changes much less for the tibia.
note: the contact point does change for the tibia (see Kinematics section) and you can make changes to the tibial slope that only affect the flexion gap. This is a more technically advanced concept. The anterior tibia is the major contact point during extension, and the posterior tibia is the major contact point during flexion, and therefore, if you increase the tibial slope you can actually increase the flexion gap and not the extension gap thru the tibia cut alone.)
It is also important to establish proper rotation of the tibial component. A good landmark for rotation is to align the anterior aspect of the tibial component with the medial 1/3 of the patellar tendon. If the tibial component is internally rotated, the tibia bone is now relatively externally rotated compared to the femur, which will rotate the tibial tubercle laterally, and thus increase the Q angle and increase risk for dislocation.
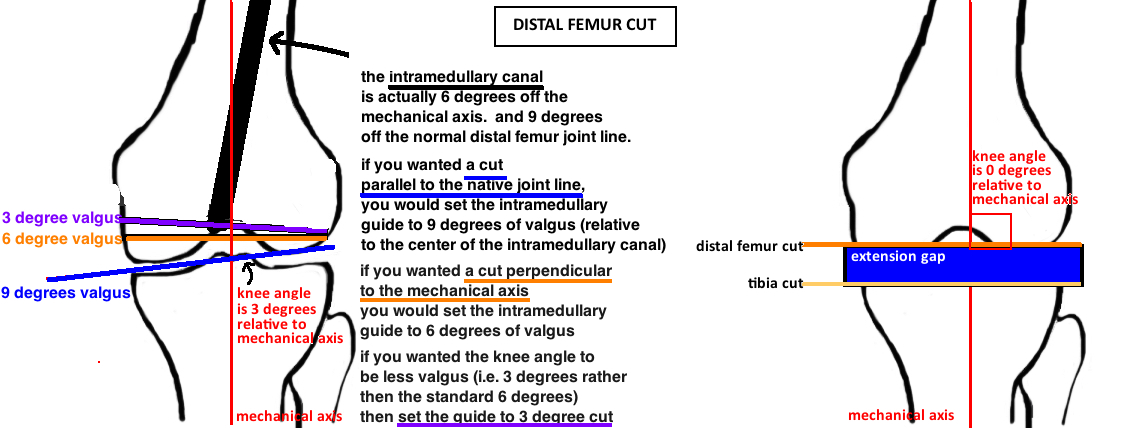
2. Distal Femoral CUT
When you cut the Distal Femur you are affecting 3 things: 1) Mechanical Alignment; 2) Extension gap; 3) the Joint Line Height
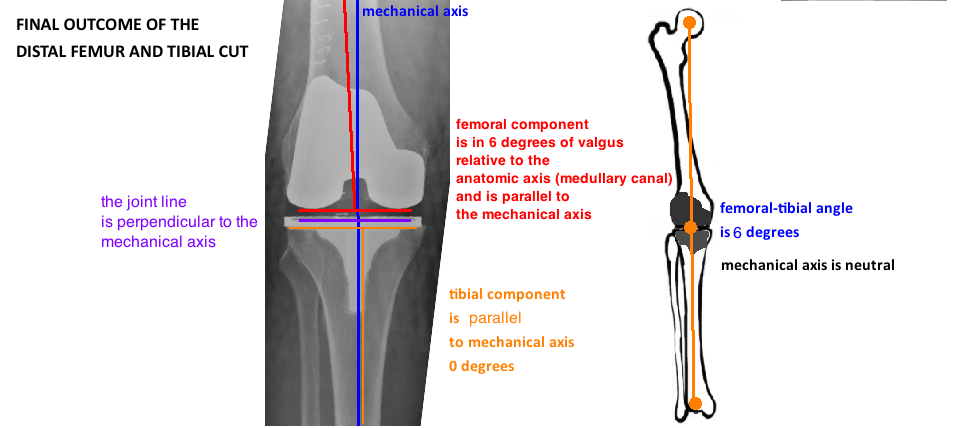
Mechanical Alignment. The goal is to place the TKA in neutral mechanical alignment. The knee is typically in neutral mechanical alignment when the "knee angle" (tibio-femoral angle) is 6° valgus. The tibial is cut at 0° relative to both the mechanical axis and the anatomic axis (they are parallel). The femur is classically cut based on an intramedullary referencing system that is guided by the medullary canal which is the same as the anatomic axis. The difference between the anatomic axis and the mechanical axis is about 6°, and that is commonly what the guide is set to. The exact measurements should be calculated preoperatively as part of the templating.
Extension Gap. If bone cuts are done correctly (0 for tibia and 6 for femur), the tibia and distal femoral cuts should be parallel to form a nice rectangle, indicating a balanced extension gap. If the gap is trapezoidal, it indicates soft tissue imbalance that requires adjustment (discussed later).
Joint Line. The femoral implant of every company... the depth of the distal femur is 9 mm (and thats is also consistent for every femoral implant size: 1 - 10...small, medium, and large...a larger femoral implant does not affect the size of the distal femoral condyle). Therefore the target depth for the distal femoral cut is 9 mm. You will take 9 mm of bone and replace it with 9 mm of metal.
note: there are exceptions. Sometimes surgeons will intentionally change the depth of the distal femoral cut. If there is a significant flexion contracture, resecting more distal femur will enlarge the extension gap (without affecting the flexion gap) and will allow more knee extension. However, every time you change the distal femur cut, you are also affecting the joint line. If you take a little extra bone form the distal femur, you raise the joint line...the implant will always be 9 mm, so if you cut 11 mm and replace it will 9 mm of metal, you have raised the joint line 2 mm. In contrast, if you take extra bone from the tibia, ie 11 mm, you can insert a bigger poly, ie an 11 mm instead of a 9 mm, and thus the joint line is not affected. The difference is that there are many sizes of poly but there is only one size for the distal femoral condyle of the implant: 9 mm. Importantly, some surgeons will also take less then 9 mm of bone from the distal femoral cut. If there is significant bone loss, then taking less bone will restore the normal joint line. If there is a pre-existing "patella baja" (ie the joint line is too high relative to the patella), then taking 7 mm of bone, and adding the 9 mm of metal, will lower the joint line by 2 mm.
3. Anterior & Posterior Femoral Cuts (FLExion gap, rotation)
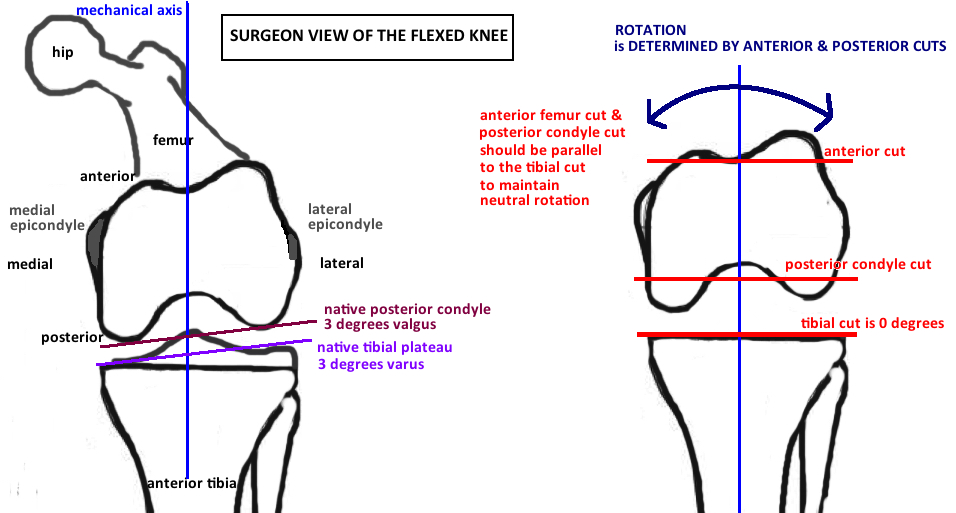
The knee is flexed and you are looking at an axial view of the distal femur. The Anterior Cut is thru the trochlear groove and the depth of this cut affects the patellofemoral joint. The Posterior Cut is thru the Posterior Femoral Condyles and it affects the flexion gap. The Anterior and Posterior Cuts are parallel and together they determine the rotation of the femoral implant.
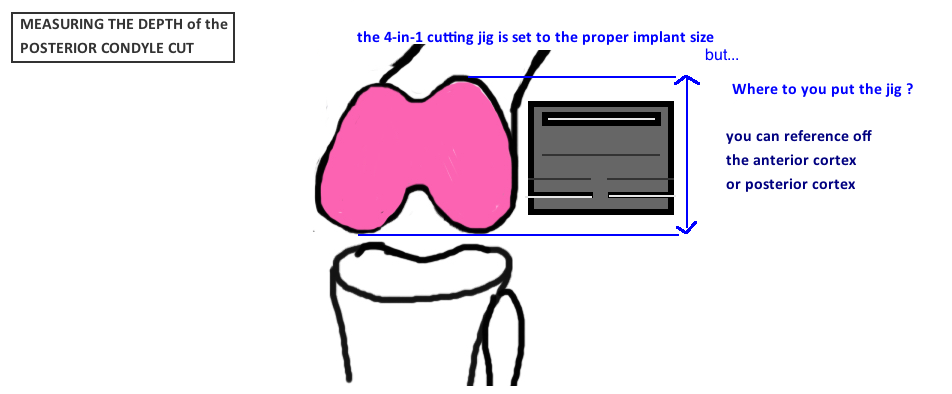
Before making these cuts, the Implant Size must be determined with a sizing guide (see picture). The anterior femur cut, the posterior femur cut, the anterior chamfer cut, and the posterior chamfer cuts are all made through the appropriately-named "4-in-1 cutting guide". There is a 4-in-1 cutting guide for each size femur. Therefore, you first get the size, then you figure out where to put the guide on the distal femur...this is what determines both rotation and flexion gap.
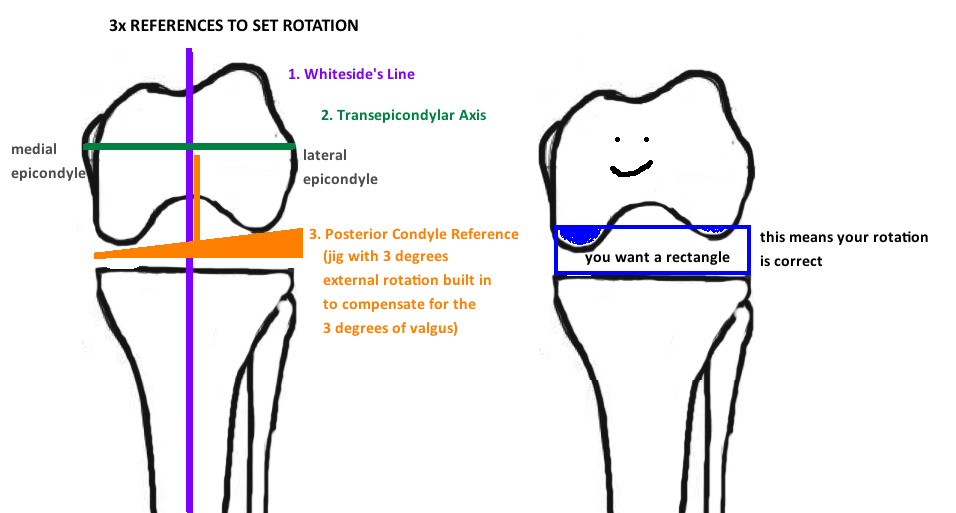
Rotation. With the knee in flexion, you are looking at an axial view of the distal femur. Rotational change occurs this axial plane, and the angle of the anterior and posterior cuts, relative to the horizontal, determines rotation. The tibia was cut perpendicular to the mechanical axis, therefore, to maintain neutral rotation in flexion, the posterior femoral cut should be parallel to this tibial cut to create a Rectangular Flexion Gap.
However, in the native knee, the posterior femoral condyles are not equal size and therefore a line across them is not parallel to the tibial cut, rather they are in 3° of valgus (to match the native tibial plateau angle of 3° varus). You therefore cannot place a flat jig under the posterior femoral condyles to obtain a neutral rotation (it will cause your cuts to be internally rotated by 3°). Instead you can take a jig that has 3 ° of external rotation dialed into it as compensation, and place it under the posterior femoral condyles to obtain a neutral rotation. Alternatively, you can use other landmarks to orient the cutting jig to obtain neutral rotation. Whitesides line is a vertical line parallel to the mechanical axis, or the Transepicondylar Axis Line (line connecting the medial and lateral epicondyles) is a horizontal line that is perpendicular to the mechanical axis. Use one of these 3 techniques to obtain a neutral rotation.
clinical correlation. Neutral Rotation is particularly important for TKA because it affects patellar tracking. Internal rotation of either the femoral or tibial component causes patellar maltracking. Mild Internal Rotation of 1-4° causes some lateral patellar tilt/tracking; Moderate Internal Rotation of 5-8° causes patellar subluxation and pain; Severe Internal Rotation > 8° can cause dislocation and failure.
Malrotation also affects the flexion gap. If you internally rotate the femur, it causes too much bone to be taken off the lateral condyle and too little taken off the medial condyle, leading to a tight medial side and loose lateral side.
Flexion Gap. Once rotation is obtained, the next step is to determine the depth of the Flexion Gap. Not only does the Flexion Gap need to be rectangular (indication of rotation), but it also needs to be the same size at the Extension Gap. Remember that the Extension gap was 9 mm. That is the target of the Flexion Gap too. Therefore, we are trying to take about 9 mm of bone off the posterior femoral condyles.
The simple way to do this is by Posterior Referencing. The jig is rigid in its position from the posterior femoral condyles. This distance is strictly 9 mm, so you will cut 9 mm off the posterior femoral condyles regardless of the jig size that you use. A smaller jig will take more bone off the anterior cortex cut, and 9 mm off the posterior cortex cut. A bigger jig will take less bone off the anterior cortex cut, and 9 mm off the posterior cortex cut. So the feet of the jig are set up against the posterior femoral condyles, and you mark this spot with two pins, then put the 4-in-1 cutting guide (for the determined implant size) onto these two pins and start cutting.
The benefit of this technique is that you recreate the normal Posterior Condyle Offset. The posterior condylar offset is important because its directly related to the arc of motion before impingement occurs (see knee kinematics). Restoration of offset allows for a normal arc of motion…yet reduced offset shifts the posterior femoral cortex closer to the posterior tibia and impingement occurs early, and this decreases knee flexion.
The thickness of the anterior cortex is variable with the posterior referencing. If incorrectly sized, and the femoral component is measured “too big”…then the anterior cut is too shallow, not enough bone is taken and so its replaced with a lot of metal, which will “overstuff” the patellofemoral joint. The patellofemoral joint becomes too tight in flexion, causing knee stiffness in flexion. If the femoral component is incorrectly sized to be “too small”
… then the anterior cut is too deep, and will cause “notching”, and may increase risk for periprosthetic fracture.
The alternative is to use Anterior Referencing. This technique is effectively the opposite of posterior referencing, whereby you directly measure the depth of the anterior cut using a boom that sits on the anterior cortex and you place two pins which will hold the 4-in-1 cutting jig.
The benefit of this technique is that your anterior depth will be great (no notching, no overstuffing).
The potential problem is that the posterior femoral condyle cut will be more variable based on how well the patient's femur anatomy matches the implant sizes. If the femur is big relative to the size of the 4-in-1 guide, you will end up removing too much bone posteriorly, which will decrease the Posterior Condyle Offset and may reduce range of motion. If the femur is small relative to the 4-in-1 guide, you will remove too little bone, and the Flexion Gap will be small relative to the extension gap.
Once the 4-in-1 cutting guide is properly oriented in depth and rotation, time to blast away.
4. PatellaR RESURFACING
Its important to recognize that patellar resurfacing is not required in knee replacements and not the standard in many countries (full controversy here). Patellar resurfacing is the standard in the United States. So lets look at the technical considerations.
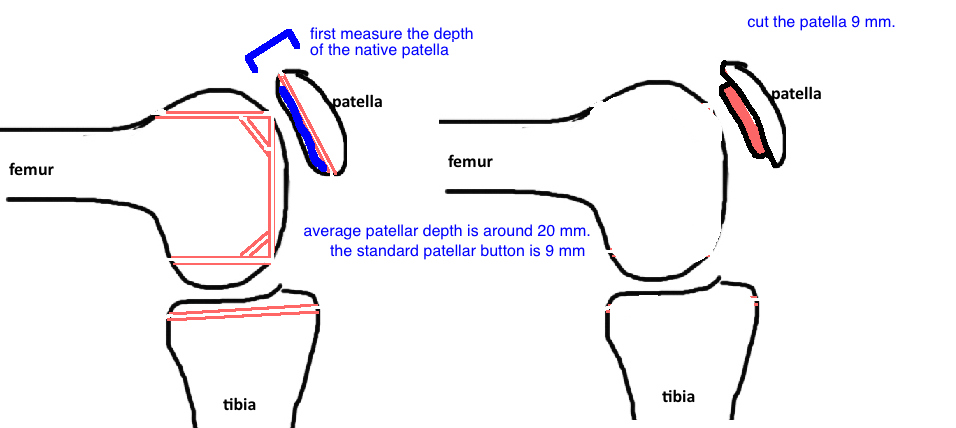
Across most device companies, the standard thickness of the Patellar Button is 9 mm. The standard patellar cut should thus be 9 mm. Measure the depth of the native patella, subtract 9 mm, and then set the patellar cutting guide to that number (if the average patellar depth is 20 mm, the patellar cutting guide is set to 11-12 mm, although many surgeons set it to 14 mm to avoid cutting the patella too thin).
Its important to avoid cutting the patella too thin because there is an increased risk of fracture when the patella is cut to < 12 mm of native patella. The standard prosthetic design has 3-pegs because there is a lower risk of fracture compared to the single peg design.
5. Cutting for Kinematic Alignment
The approach to the bone cuts for kinematic alignment is slightly different because the goal is to maintain the native joint line.
The distal femoral cut is made using an intramedullary cutting guide that is parallel to the distal femur joint line (which is 3° valgus). The posterior femoral cut is made using the posterior reference system that is set to 0° rotation (unlike the mechanical alignment which is set to 3° of external rotation) so it is in direct contact with both posterior condyles.
The tibial cut is more challenging. The axis of neutral rotation needs to be established before making the tibial cut. This is because the cut is 3° of varus (not 0° as in the mechanical alignment approach) and therefore, cutting this "off-plane" will cause abnormal kinematics. The tibia is then cut in slight varus.