Correct alignment of the TKA implant is critical to restoring function and maximizing longevity. TKA Malalignment is associated with early loosening (due shear stresses at the bone-implant interface), accelerated poly wear (due to uneven stress distribution), and increased pain (due to abnormal stresses on the surrounding soft tissue envelope).
However, there are two schools of thought regarding the target of TKA implantation: 1) Mechanical Axis Alignment and 2) Kinematic Axis Alignment (also referred to as Anatomic Alignment).
1. Mechanical Alignment
The goal of TKA alignment is to restore the normal mechanical axis. This is not achieved however by attempting bone cuts that recreate the exact joint line between tibia and femur, which would be 3° tibial varus and 3° femoral valgus in the native knee. Instead, both the distal femur and the tibia are cut to be perpendicular (0°) to the mechanical axis.
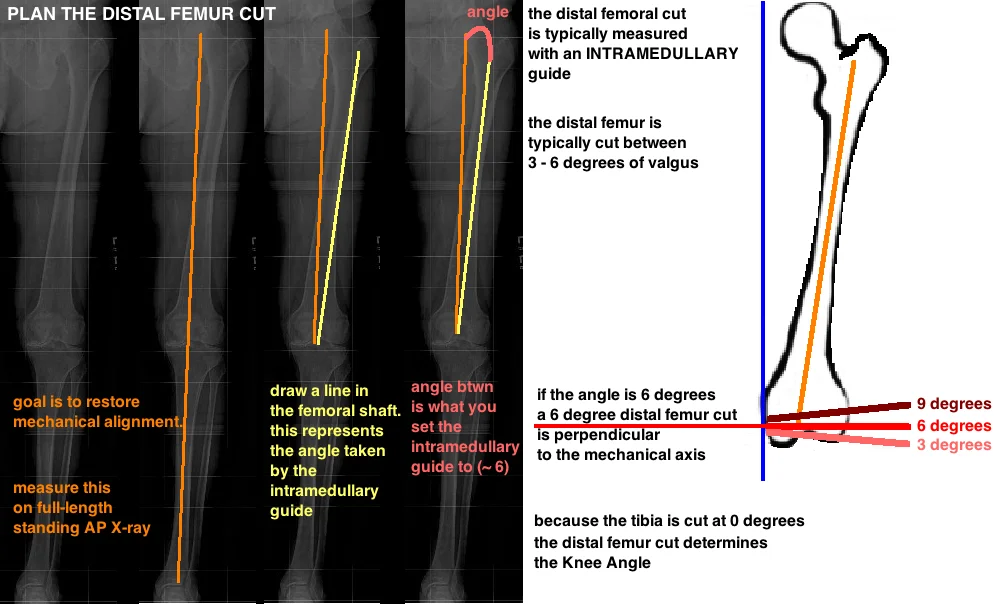
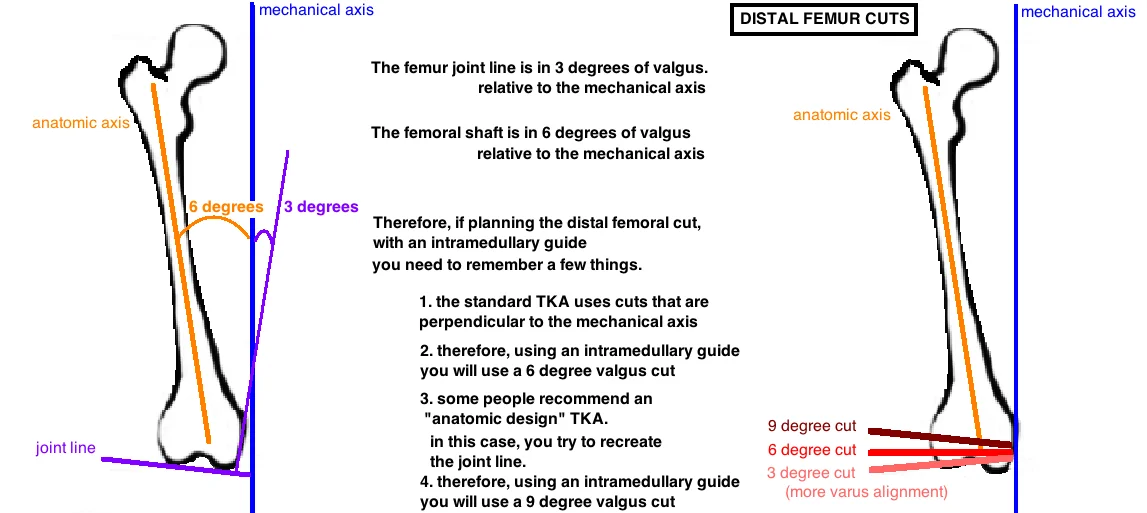
The femur cut ("distal femoral cut") uses an intramedullary guide based on the anatomic axis. The angle of the medullary canal (anatomic axis) is used to determine the angle of the cut, and therefore, the angle of the joint line (around 3°) can be pretty much ignored here.
Lets look at it again with a different diagram.
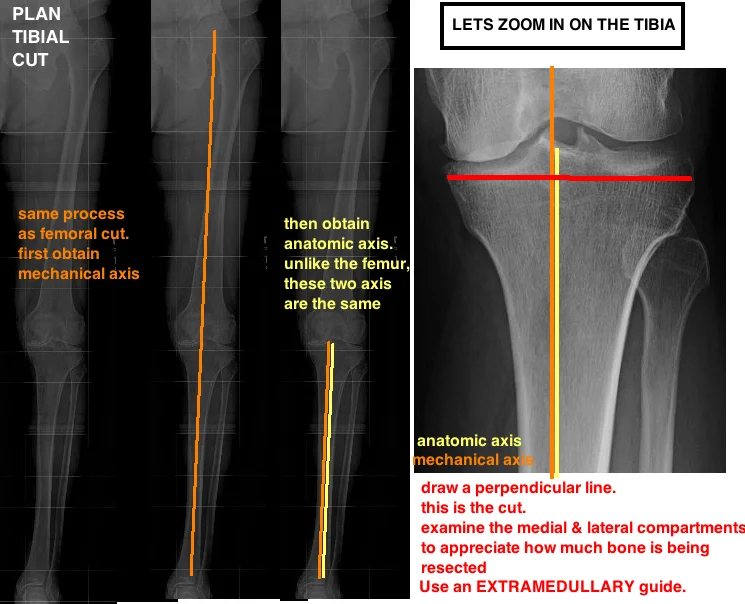
The tibial cut is a little more straight forward because the mechanical axis and the anatomic axis are the same.
The tibia is cut at 0° (perpendicular to mechanical/anatomic axis), while the native tibia joint line is in slight varus (roughly 3°). This means that we are over-resecting the lateral side (anatomically the lateral side is slightly higher giving that 3° varus, so with a cut at 0° you are resecting slightly more lateral tibia).
Theoretically over resecting lateral tibial bone causes some varus laxity. You can compensate by performing a medial release of soft tissue (such as taking down some of the deep MCL); or adjust the bony cuts on the femoral side by a) under-resect the lateral distal femur (decrease the valgus angle slightly to 6° based on the intramedullary femur guide... instead of cutting the femur at 9°) to reconcile the extension gap, and b) balance the flexion gap by adding 3° of external rotation (this technique was originally implemented to compensate for the tibial cut…and the improved patellar tracking is just an added bonus). Thus, the femoral cuts reflect a slight variation from the anatomic ideal as compensation for the tibial cut.
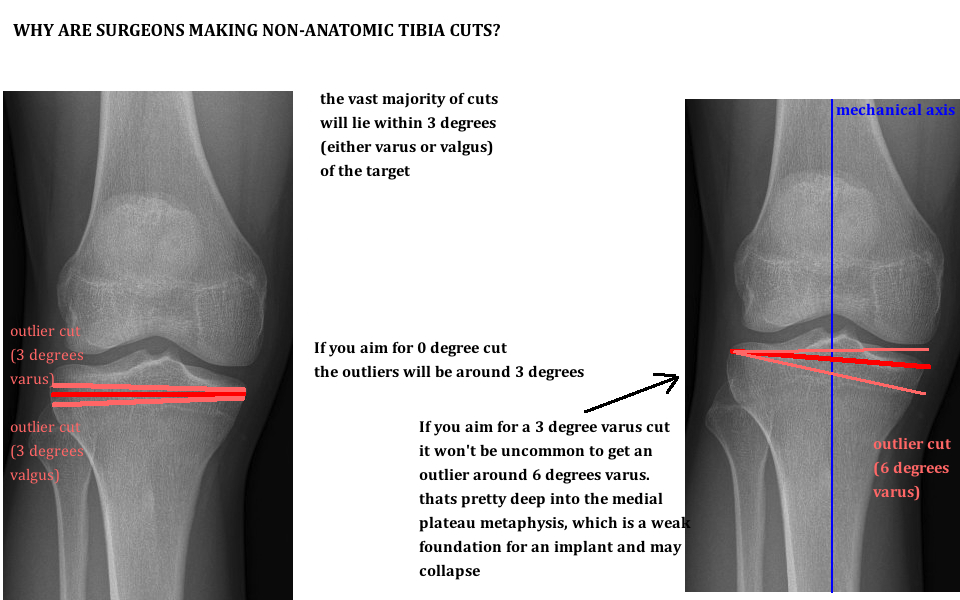
The big question here is why change the tibia cut to begin with? If the non-anatomic tibia cut leads you down this path of compromise and compensation, why not just cut the tibia in 3° of varus? Basically surgeons are hedging. We operate in the real world, and our cuts aren't always perfect. Studies have demonstrated we can expect up to 3° error (either varus or valgus) in 30% of tibial cuts. If 0° is the target of our tibial cut, then variations off that target (3° varus to 3° valgus) still allow for stable implants. In contrast, if 3° varus is the target tibial cut and the error range remains 3°, then implants will be regularly inserted with up to 6° of varus. Too much varus shifts the mechanical axis away from the center of the knee toward the medial compartment. Too much varus also causes a deeper medial cut, exposing excess cancellous bone to abnormally high forces. The medial metaphyseal bone gets abruptly weak when the implant sits >10 mm below the joint line. If too much stress is placed onto the medial tibial plateau, there is added risk of medial sided collapse and aseptic loosening. Therefore, the designing surgeons recognized the inherent error rate and decided to make the target a safer angle of 0°. The non-anatomic cuts in TKA are performed to maximize the number of stable implants.
2. Kinematic Alignment
Some surgeons think that mechanical axis is important, but restoring anatomic alignment around the knee is more important. They believe that all of the non-anatomic cuts made to the femur and tibia have a cumulatively detrimental impact on postop TKA function. Therefore, they cut the femur in 9° valgus and the tibia in 3° varus to re-establish the normal joint line.
Proponents of this technique argue that despite older studies showing that over 3.9° of tibial varus leads to increased failure, recent studies on kinematic alignment of the tibia at 3 and 6 years show no evidence of adverse effect of tibial positioning [1, 2] [3-5]. Furthermore, when comparing kinematic and mechanical alignment approaches, both show similar mechanical angle (hip-knee-ankle) and knee angle, with the femur being cut on average with 2° more valgus and the tibia with 2° more varus. [6].