Over 50,000 revision TKA are performed in the USA every year and this number is growing as patients are living longer. Its projected to rise up to 6x by 2030. The most common reasons for revision include aseptic loosening (28%), septic loosening (14%), pain without known etiology (9%).
There are 4 key issues with a revision TKA. 1) Getting Exposure. 2) Obtaining Stability. 3) Addressing Bone Loss; 4) Restoring the Joint Line.
Getting Exposure
Approach. Evaluate skin quality and prior incisions. Principles of skin blood supply should be maintained. Arthrotomy may require a more extensile exposure if knee is stiff. The Quad Snip or Tibial Tubercle Osteotomy effective mobilize the extensor mechanism to expose the joint.
Extensile Exposures for Revision TKA
Mobilization. The knee in extension allows for evaluation of the medial and lateral gutters, which often require fibrous debulking to give sufficient flexion and extension (be careful not to damage the collateral ligaments). Trying to forcefully flex the knee puts the patellar tendon at risk. Additionally, try to avoid patellar eversion due to risk of tendon avulsion (if this is a significant concern, place a pin into the medial side of the tendon as a piton).
Implant removal. A good preop plan is necessary to predict difficulties. Know the implants being removed. Predict if implants are fixed or loose, but have removal tools available regardless. There is a sequence of removal that optimizes visualization.
1. Remove poly. Use narrow curved osteotome to disengage from the tray.
2. Remove femoral component. Removing implants without removing too much bone is the biggest challenge. Aim the osteotome at the the implant-cement (not cement-bone) interface. If already loose, place impactor over the anterior flange.
3. Remove tibial component. Must be able to hyperflex knee to clear the posterior-lateral tibial condyle.
Re-implantation.
Bone Loss.
Cones or sleeves are used to compensate for metaphyseal bone loss. If the metaphysis is completely gone then a proximal tibia or distal femur replacement may be required. Augments along the distal femur or posterior femur (sizes 5, 10, 15 mm) can be used on the femoral implant to build up the areas of bone loss (cement cannot be used reliably to fill bone defects > 5 mm. Stems should be used if augments or cones are required to increase contact area between implant and good bone.
Stability.
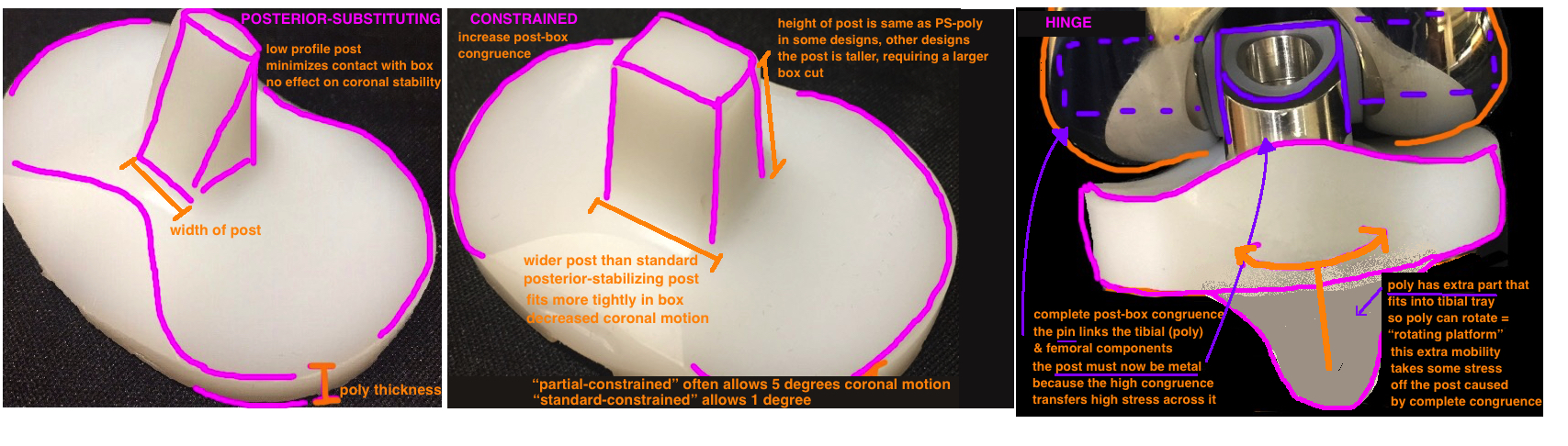
Constrained implants or hinged implants may be needed if there is ligament insufficiency.
Increasing TKA constraint occurs by Increasing the congruity between Tibial Post and Femoral Box
Restoring the joint line.
This key to obtaining good postoperative motion. Patella baja is the most common risk.
Evaluate the preoperative x-rays for signs of patella baja caused by scarring of the patellar ligament, or subsidence of femoral component secondary to osteolysis or fracture. Distal femoral bone loss must be replaced with augments to prevent baja. Using a larger poly to fill big extension gap caused by femoral bone loss will cause Patella Baja. The length of the femur is shortened by the bone loss, while the length of the proximal tibia is increased by the large poly. For example, if you remove 14 mm of distal femur and place a primary femur implant (remember all primary TKA have 9 mm of metal to replace the distal femur bone), then you’ve moved the joint line up by 5 mm, so the patella is now 5 mm lower in relation to the raised joint line. This should be corrected by placing 5 mm augments on distal femur portion of the implant (remember augments to the distal femur will affect the extension gap only, not the flexion gap).
Intraoperatively, you can identify baja if the inferior pole of the patella is touching the poly with the knee in extension. The inferior pole of the patella should be sitting in the trochlear groove.
Radiographic measures to determine the position of the joint line. The Insall-Salvati Ratio can describe the relative position of the patella by measuring the distance between the distal pole of the patella to the proximal tibia divided by the length of the patella itself. The denominator (the patellar length) is constant. The distance of the patella from the tibia (the patellar tendon length) is variable. If patella is sitting too close to the tibia, its sitting too low, and therefore its Baja. There are other generalizable radiographic criteria. The Joint line is 10 mm above the fibular head, 25 mm below the lateral epicondyle, and 35 mm below the medial epicondyle.
Radiographic measurements of the Joint Line