Bone loss is a major challenge with revision THA (particularly cases of osteolysis and infection). Bone loss means less bony coverage of the cup which means less surface area for ingrowth which means higher risk for failed fixation of the cup.
Bone loss can also compromise initial stability. A primary THA utilizes hoop stress of an intact acetabular rim to give stability for a press-fit implant (the press-fit is the primary source of implant stability until ingrowth occurs around 6 weeks). The standard titanium cup designs require micromotion < 50 μm, and about 50% contact between the implant and viable bone for successful ingrowth [1] . New porous metals, such as trabecular metal, have been developed for the revision setting where initial stability and bony ingrowth is a challenge. This technology increases friction between the implant and bone, increasing initial stability despite less bony contact, and it encourages extensive rapid bone ingrowth [2].
Bone defects can be described as “segmental” or “cavitary”. “Segmental” refers to defects of the acetabular rim, which compromises stability, because only an intact rim can withstand the hoop stresses that stabilize a press-fit cup. “Cavitary” refers to volumetric bone loss where the rim remains intact. Both however decrease coverage of the implant [3].
X-rays are used to determine the type and location of bone loss. This is achieved by looking for lysis at the ischium, teardrop and determining if the hip center has migrated superior, medial or lateral. Judet views ("O.A.K" Obturator Oblique shows Anterior "K"olumn, Posterior Wall, Iliac Oblique shows Posterior Column, Anterior Wall) and a CT scan of the pelvis can be used to further characterize bone loss.
- Superior migration of the hip center indicates bone loss at the dome. If you identify superior migration, then determine if its Superior + Medial (indicating anterior column > posterior column bone loss) or Superior + Lateral migration (indicating posterior column > anterior column loss).
-Isolated medial migration ("protrusio") of the hip center is a defect in the anterior wall identified on x-ray as a break in the ilioischial line ("Kohler's line").
- Lysis. Osteolysis of the ischium reports posterior column/posterior wall involvement. Osteolysis of the teardrop indicates inferior bone loss. Break in ilioischial line indicates anterior column bone loss.
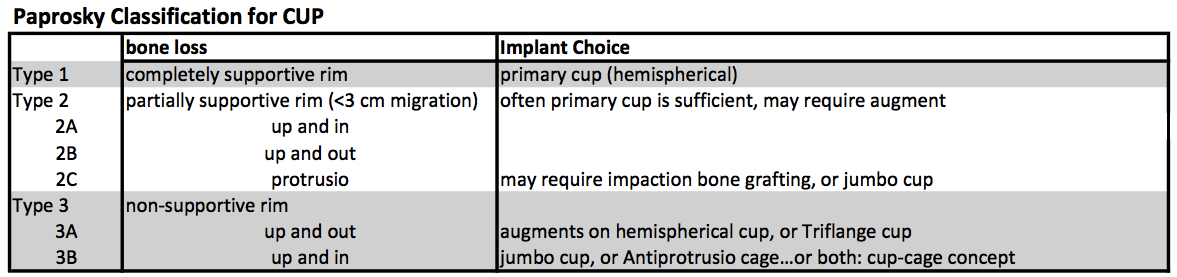
The Paprosky Classification was established to further characterize the severity of bone loss, which in turn guides treatment (different grades of bone loss require different implants to achieve stability) [4]. Lets look first at the Classification, and then at the corresponding treatment options.
Type 1. Standard hemispherical cup is sufficient to get stability because the rim is completely supportive.
Type 2. Stable Rim but only partially supportive, meaning it may have some disruption (segmental defect) without compromising overall stability. The key is that migration is not significant, and often a hemispherical cup is sufficient to achieve stable fixation, although an augment may be used to improve contact area for ingrowth.
Type 3. The hallmark of Type 3 is an unsupportive rim. Thus a hemispherical cup cannot be used to achieve initial fixation. This type is then separated into A and B.
Type 3A is a posterior column/wall defect. The hip center migrates “up and out” (superior lateral migration > 3 cm).
Type 3B is an anterior column/wall defect (which has a higher association with pelvic discontinuity). The hip center migrates “up and in” (superior medial migration > 3 cm). In a Type 3B, the surgeon must first determine if pelvic discontinuity is present before addressing the acetabular defect (otherwise the acetabulum will continue to open up and the cup will never achieve stable fixation).
If discontinuity is present, the options are a cage, a cup-cage, a custom triflange, or a distraction technique.
Revision Cups
▪ Augments on a Hemispherical cup is required when the rim is not intact. Titanium augments improve surface area of bony contact for ingrowth. Augments are becoming more popular as multiple configurations are available, such as the “flying buttress” for superior placement, or a “dome” augment for rim defects anywhere, and also the “footing” augment for medial defects. [5]
▪ Triflange cup can also be used when the rim is not intact. Some cases of pelvic discontinuity can be addressed with a Custom Triflange cup, modeled based on CT imaging of the pelvis. The implant contains locking screws to the ischium (inferiorly) and ilium (superiorly) for initial fixation, and its custom shape allows for sufficient bony contact for long-term stable fixation.
▪ Jumbo Cup. In cases of large cavitary defects (contained lesions with < 50% bone contact), a Jumbo Cup is used (defined as outer diameter >66 mm). The Jumbo Cup is coated with highly-porous metal (ie Tantalum or Trabecular Metal) and provides better fixation via improved biocompatibility for host osteoblasts to ingrow. These highly-porous metal additionally have a high coefficient of friction, and elasticity to give better initial fixation [6] [7].
▪ Antiprotrusio Cages (“cage”) were used historically as the workhorse for pelvic discontinuity and to treat large contained lesions. The cage spans a large bone defect, and stability is achieved through proximal screw fixation to the ilium (superiorly) and engaging the ischium (inferiorly). A poly liner is then cemented into the cage. Because cages never achieve biologic fixation, there is a risk of fatigue failure [8], with failure rates around 20-30% at 5 years. The cage fails via abduction pull out.
▪ Cup-Cage Concept is way to combine the benefits of both jumbo cups and cages [9]. The Cup-Cage technique inserts a "jumbo" trabecular metal shell (>60 mm) into the defect and adds fixation with multiple holes thru the cup into the acetabulum. Then a cage (described above) is inserted on top of the cup and fixation is achieved with screws into the ilium and a slotted flange into the ischium. The cage further stabilizes the acetabulum to minimize micromotion and promote ingrowth. A poly liner is then cemented into the cage. The advantage of this technique is that it provides excellent immediate fixation (via cage) while also allowing for long-term biologic fixation (via jumbo cup). Good outcomes are reported for Cup-Cage technique [10]. It can also be used in Type 3A and 3B defects (with and without pelvic discontinuity) which still have significant bone loss making long-term fixation a challenge [11, 12].
Beyond bone loss, Instability is major challenge with revision THA, and it can be partially addressed through the choice of implants (for full discussion see Instability, in the Complications Section). The femoral head can be upsized to increase jump distance and arc of motion before impingement. The poly liner can provide increased version or increased jump distance, or it can be constrained.
References
1. Pilliar, R.M., J.M. Lee, and C. Maniatopoulos, Observations on the effect of movement on bone ingrowth into porous-surfaced implants. Clin Orthop Relat Res, 1986(208): p. 108-13.
2. Deirmengian, G.K., et al., Management of acetabular bone loss in revision total hip arthroplasty. J Bone Joint Surg Am, 2011. 93(19): p. 1842-52.
3. D'Antonio, J.A., et al., Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res, 1989(243): p. 126-37.
4. Paprosky, W.G., P.G. Perona, and J.M. Lawrence, Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty, 1994. 9(1): p. 33-44.
5. Sporer, S.M., How to do a revision total hip arthroplasty: revision of the acetabulum. J Bone Joint Surg Am, 2011. 93(14): p. 1359-66.
6. Welldon, K.J., et al., Primary human osteoblasts grow into porous tantalum and maintain an osteoblastic phenotype. J Biomed Mater Res A, 2008. 84(3): p. 691-701.
7. Bobyn, J.D., et al., Characteristics of bone ingrowth and interface mechanics of a new porous tantalum biomaterial. J Bone Joint Surg Br, 1999. 81(5): p. 907-14.
8. Sembrano, J.N. and E.Y. Cheng, Acetabular cage survival and analysis of factors related to failure. Clin Orthop Relat Res, 2008. 466(7): p. 1657-65.
9. Hanssen, A.D. and D.G. Lewallen, Modular acetabular augments: composite void fillers. Orthopedics, 2005. 28(9): p. 971-2.
10. Kosashvili, Y., et al., Acetabular revision using an anti-protrusion (ilio-ischial) cage and trabecular metal acetabular component for severe acetabular bone loss associated with pelvic discontinuity. J Bone Joint Surg Br, 2009. 91(7): p. 870-6.
11. Paprosky, W.G., M. O'Rourke, and S.M. Sporer, The treatment of acetabular bone defects with an associated pelvic discontinuity. Clin Orthop Relat Res, 2005. 441: p. 216-20.
12. Della Valle, C.J., et al., High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty, 2005. 20(7 Suppl 3): p. 103-7.